When a person living with HIV starts an antiretroviral regimen that includes Efavirenz is a non‑nucleoside reverse transcriptase inhibitor (NNRTI) widely prescribed for its potency and once‑daily dosing, the next question often isn’t just about viral suppression. It’s about what the drug means for future pregnancies, birth outcomes, and everyday contraceptive choices. Below you’ll find the facts you need to weigh the benefits against the reproductive risks, how to counsel patients effectively, and what the latest guidelines say.
Why Efavirenz Still Matters in Modern HIV Care
Efavirenz remains a pillar of first‑line HIV therapy in many low‑ and middle‑income countries because it’s inexpensive, has a high barrier to resistance, and fits well into fixed‑dose combinations. The World Health Organization (WHO) still lists it as a preferred component of the Antiretroviral therapy (ART) backbone for adults. However, its neuropsychiatric side effects and potential teratogenicity keep clinicians on alert, especially when patients are of reproductive age.
Efavirenz and Pregnancy: What the Data Show
Early animal studies raised red flags about neural tube defects, prompting a worldwide caution label. Human data collected over the past two decades tell a more nuanced story. Large cohort analyses from the United States, Europe, and sub‑Saharan Africa indicate that the absolute risk of major congenital anomalies remains low-around 1‑2%-and is not statistically higher than in the general population when efavirenz is taken after the first trimester.
- First‑trimester exposure: most guidelines recommend avoiding efavirenz if conception is planned or confirmed.
- Second‑ and third‑trimester exposure: studies show no significant increase in birth defects, but close monitoring is advised.
- Maternal viral load: staying suppressed throughout pregnancy is the strongest predictor of a healthy baby.
In practice, the key takeaway is to avoid efavirenz during the first 12 weeks of pregnancy whenever possible, but the drug can be continued safely later if the benefits outweigh the uncertainties.
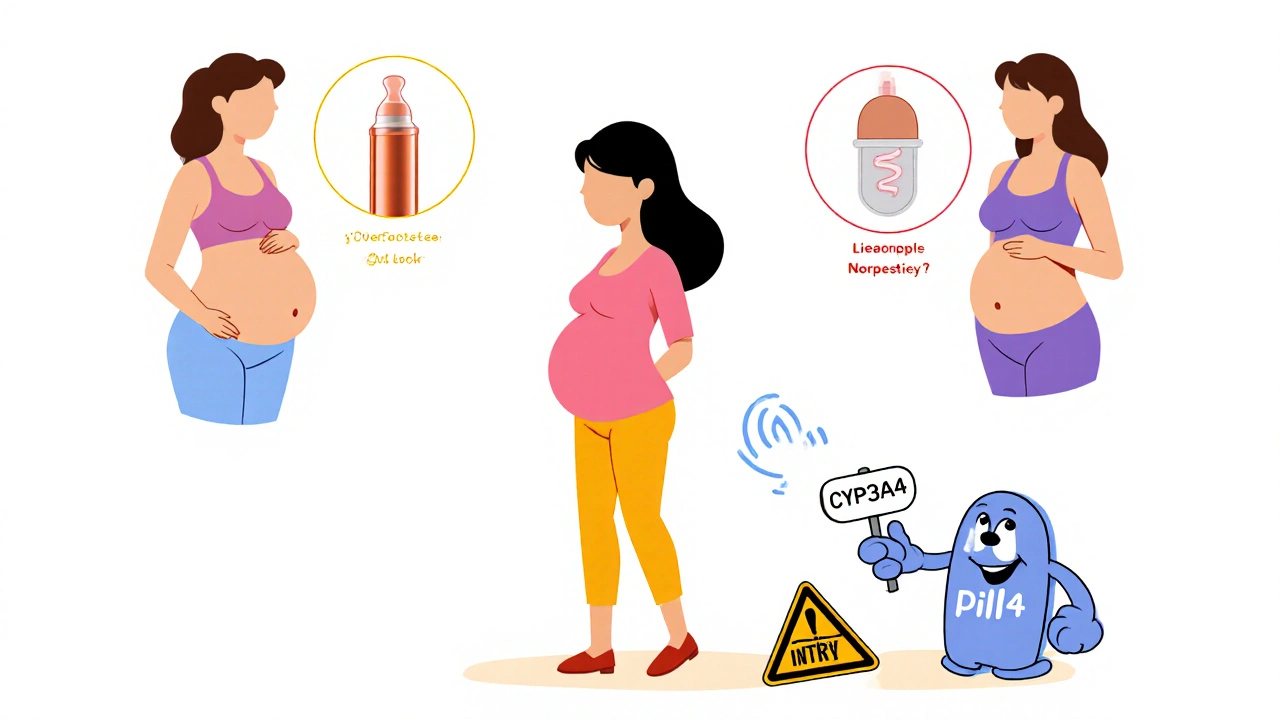
Contraception Considerations for Women on Efavirenz
Efavirenz induces the enzyme CYP3A4, which can lower the effectiveness of hormonal contraceptives that rely on this pathway. The result is a higher chance of breakthrough bleeding and, more importantly, unintended pregnancy. Here’s how to navigate the interaction:
- Prefer contraception methods that are not metabolized by CYP3A4: copper IUDs, levonorgestrel IUDs, and the progestin‑only implant are reliable choices.
- If a combined oral contraceptive (COC) is preferred, choose a formulation with a higher estrogen dose (30‑35µg) and consider adding a barrier method.
- Discuss the timing of efavirenz initiation relative to contraceptive start dates to minimize overlap during the enzyme induction period (roughly 2‑3 weeks).
Clinicians should document the chosen method, counsel on backup options, and schedule a follow‑up visit within one month to assess adherence and side effects.
Breastfeeding While on Efavirenz
Breastfeeding offers critical nutrition and immunity benefits, especially in resource‑limited settings. Efavirenz passes into breast milk at low concentrations-approximately 0.5% of maternal plasma levels. The WHO recommends that women on efavirenz can breastfeed safely if the infant is HIV‑negative or receives appropriate prophylaxis.
- Monitor infant growth and HIV status at regular intervals (6 weeks, 3 months, 6 months).
- Educate mothers on signs of drug‑related toxicity, though these are rare.
- Encourage exclusive breastfeeding for the first six months, then gradual weaning while maintaining maternal ART.
In high‑income countries where formula feeding is an option, the decision often hinges on patient preference and access to clean water.
Comparing Efavirenz with Other NNRTIs on Reproductive Safety
| Drug | First‑trimester risk | CYP3A4 interaction | Breastfeeding safety |
|---|---|---|---|
| Efavirenz | Potential neural‑tube risk; avoid if possible | Strong inducer - reduces hormonal contraceptive levels | Low milk transfer; considered safe with monitoring |
| Nevirapine | No clear teratogenic signal | Weak inducer - minor effect on contraceptives | Safe; higher milk concentrations but no adverse infant outcomes reported |
| Rilpivirine | Limited data; no known increased risk | Minimal interaction - compatible with most hormonal methods | Data scarce; cautious use recommended |
The table highlights why clinicians may switch from efavirenz to nevirapine or rilpivirine in women planning a pregnancy, especially when hormonal contraception is the primary method.
Practical Counseling Checklist for Clinicians
Use this quick reference during a patient visit. It covers the essential points without overwhelming the conversation.
- Confirm HIV status, viral load, and CD4 count.
- Ask about pregnancy intention and current contraceptive use.
- Discuss efavirenz’s first‑trimester risk and suggest alternative regimens if pregnancy is planned.
- Review drug-drug interactions with hormonal methods; offer CYP3A4‑independent options.
- Explain breastfeeding benefits and efavirenz’s low milk transfer.
- Provide written handouts that summarize key dates (e.g., 2‑week enzyme induction window).
- Schedule follow‑up within 4 weeks to reassess adherence and side effects.
Document each step in the medical record; it reinforces shared decision‑making and protects both patient and provider.
Special Populations: Men, Transgender Individuals, and Adolescents
While most reproductive‑health discussions focus on cis‑gender women, efavirenz’s effect on fertility isn’t limited to them.
- Men: Efavirenz does not impair sperm parameters, but partners should still be counseled about the female partner’s contraception needs.
- Transgender women on hormone therapy: Efavirenz can lower estradiol levels, potentially affecting feminization goals. Close monitoring of hormone levels is advised.
- Adolescents: Emphasize education on safe sex, consistent condom use, and the importance of regular HIV care visits.
Tailoring the conversation to each individual’s gender identity and life stage improves adherence and outcomes.

Monitoring and Follow‑Up After Pregnancy or Conception
If a patient becomes pregnant while on efavirenz, the protocol shifts:
- Confirm gestational age with ultrasound.
- If first trimester, discuss switching to an alternative NNRTI or an integrase inhibitor, balancing the risk of viral rebound.
- Maintain viral load testing every 4 weeks throughout pregnancy.
- Coordinate with obstetrics for delivery planning; aim for a viral load < 50 copies/mL at birth to minimize transmission.
- After delivery, reassess ART regimen based on breastfeeding intentions and postpartum contraceptive plan.
Close collaboration between the HIV specialist, obstetrician, and pediatrician is the cornerstone of a healthy outcome.
Key Takeaways
- Efavirenz is effective but carries a precaution for first‑trimester exposure.
- It reduces hormonal contraceptive efficacy; opt for IUDs or implants when possible.
- Breastfeeding while on efavirenz is generally safe with proper infant monitoring.
- Alternative NNRTIs like nevirapine offer smoother reproductive‑health profiles.
- Structured counseling and regular follow‑up ensure both viral suppression and reproductive goals are met.
Frequently Asked Questions
Can I get pregnant while taking efavirenz?
Yes, pregnancy is possible, but most guidelines advise avoiding efavirenz during the first 12 weeks because of a potential, though low, risk of neural‑tube defects. If pregnancy occurs, discuss switching regimens with your provider.
Does efavirenz reduce the effectiveness of birth‑control pills?
Yes. Efavirenz induces CYP3A4, which can lower estrogen and progestin levels in combined oral contraceptives. Using a copper IUD, levonorgestrel implant, or a higher‑dose pill with a backup method is recommended.
Is it safe to breastfeed my baby while I’m on efavirenz?
The drug appears in breast milk at very low levels, and the WHO considers breastfeeding acceptable for mothers on efavirenz, provided the infant receives HIV prophylaxis and regular health checks.
What are safer NNRTI alternatives for women planning a pregnancy?
Nevirapine and rilpivirine have more reassuring reproductive safety data and weaker interactions with hormonal contraceptives, making them common alternatives when pregnancy is anticipated.
How often should my viral load be checked during pregnancy?
Guidelines suggest every four weeks throughout pregnancy and more frequently if the viral load rises above 200 copies/mL.

Hey there! Just wanted to say you did a great job pulling all that info together, and it’s super helpful for folks trying to figure out efavirenz and pregnancy. The way you broke down the contraceptive options is especially neat-makes it easy to share with patients. Keep it up, and definitely keep the tone friendly, even if some of the stats are a bit dense for laypeople. You’re definitely on the right track, definatly keep sharing!
Wow, another post telling us to trust the WHO and big pharma’s “guidelines”. As if they haven’t been tweaking the data for years to keep us hooked on cheap pills. Good thing you highlighted the neuro‑psychiatric side effects-sounds like they’re just trying to scare us off while they line their pockets. Thanks for the heads‑up, but don’t expect me to quit efavirenz without a massive conspiracy‑theory‑level debate first.
I really appreciate how thorough this overview is, especially the way you laid out the step‑by‑step counseling checklist. It’s crucial for clinicians to have a concise reference that doesn’t overwhelm patients during a stressful visit. Your emphasis on confirming pregnancy intentions aligns with what we see in real‑world practice, where the conversation often gets rushed. I also like the clear distinction between first‑trimester risks and later‑trimester safety; that nuance can make a huge difference in decision‑making. The discussion about CYP3A4 induction and hormonal contraceptive efficacy is spot‑on, and the suggested alternatives like copper IUDs are evidence‑based. Moreover, pointing out the low milk transfer rates for efavirenz helps dispel a lot of maternal anxiety around breastfeeding. The tables comparing NNRTIs provide a quick visual aid that many providers will find handy. It’s good that you mentioned both cis‑gender women and other gender identities, because reproductive health isn’t one‑size‑fits‑all. The section on adolescent counseling reinforces the need for age‑appropriate education, which is often neglected. I also appreciate the reminder to document every step in the chart; legal protection matters as much as patient care. Your recommendation for viral load checks every four weeks during pregnancy follows the latest guidelines and should improve outcomes. The backup plan of switching to nevirapine or an integrase inhibitor if a patient becomes pregnant early is a pragmatic approach. Overall, the balance of pharmacology, obstetrics, and patient‑centered communication makes this piece a valuable resource. I’ll definitely be sharing this with my clinic’s team and using it for teaching residents. Thank you for the comprehensive and compassionate synthesis. Keep updating it as new data emerges, and the community will stay informed.
Listen, you’ve got it all twisted. Efavirenz is a godsend for the American powerhouse, and anyone whining about “big pharma” clearly doesn’t understand the glorious march of our nation’s health supremacy. If you think we should ditch a drug that’s saved millions, you’re basically cheering for our rivals to take over. Drop the conspiracy babble and recognize that this regimen fuels our dominance on the global stage-no need for all that melodramatic whining.
Whoa, that deep dive was amazing! I love how you broke everything into bite‑size nuggets-makes it way less scary for patients. The checklist vibe is exactly what my clinic needs to keep things moving fast. Also, the tip about pairing higher‑dose OCPs with a barrier method is gold. Thanks for making the science feel so approachable; I’m gonna share this with the whole team.
While your patriotic fervor is noted, it does not alter the pharmacokinetic realities governing efavirenz’s interaction with hormonal contraceptives. The assertion that national dominance supersedes patient safety lacks empirical support and could jeopardize clinical outcomes. A rigorous, evidence‑based assessment remains indispensable, irrespective of ideological leanings. Therefore, the claim that efavirenz should be embraced without reservation is scientifically untenable.
It’s absolutely clear that any discussion which downplays the strategic advantage supplied by efavirenz is nothing short of sabotage. The United States has always led the charge in HIV therapy, and we must continue to prioritize drugs that keep our global influence strong. Those who whisper about “first‑trimester risk” are simply trying to undermine our national health agenda, whether intentional or not. In short, let’s stay the course and trust the established protocol, errors and all.
One thing that struck me while reading this guide is how the timing of enzyme induction could intersect with patients’ menstrual cycles, potentially affecting hormone levels beyond just contraceptive efficacy. It might be worth exploring whether scheduling efavirenz initiation during a specific phase could minimize breakthrough bleeding. Also, the data on breastfeeding exposure, while reassuring, could benefit from larger longitudinal studies in diverse populations. Overall, the piece prompts a lot of thoughtful questions that could shape future research.
Indeed, the points you raise are salient; however, it is imperative to underscore that the current literature-while extensive-still exhibits gaps, particularly regarding longitudinal breastfeeding outcomes. Moreover, the suggestion to align efavirenz initiation with menstrual phases, though theoretically plausible, lacks robust empirical validation; thus, it remains speculative at best. Consequently, any clinical recommendation predicated upon such timing must be presented with appropriate caveats, lest it mislead practitioners.
Great summary, very useful.
Let me be crystal clear: until randomized controlled trials definitively prove that timing efavirenz with menstrual cycles yields a measurable benefit, we should not divert resources into such speculative protocols. The focus must remain on proven strategies-viral suppression, reliable contraception, and rigorous monitoring. Anything less is simply a waste of time and taxpayer money.