Milk Thistle Medication Interaction Checker
Check Your Medication Risk
Select medications you're taking to see if they may interact with milk thistle. This tool is based on scientific evidence about liver enzyme interactions.
Interaction Risk Assessment
Some of your selected medications have known interactions with milk thistle. Proceed with caution and consult your doctor before taking milk thistle.
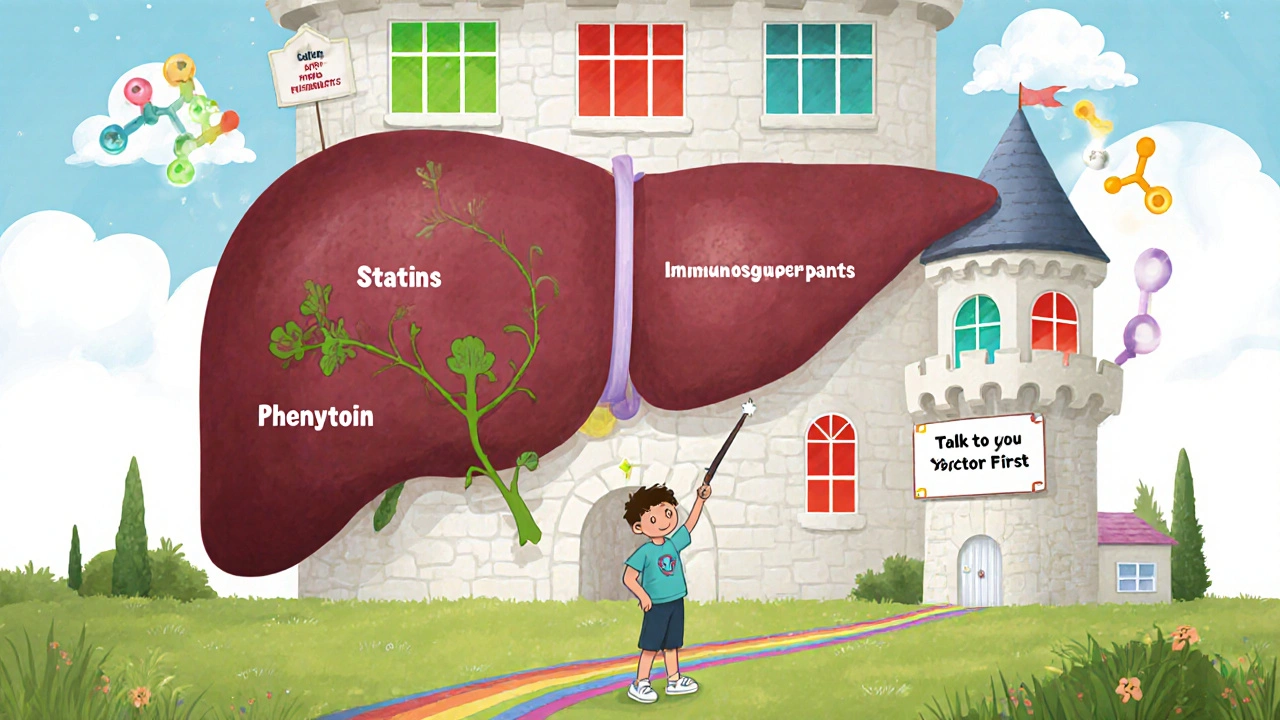
When you take milk thistle for your liver, you might think you’re just giving your body a gentle boost. But if you’re also on prescription meds-especially blood thinners, seizure drugs, or statins-you could be walking into a hidden interaction zone. It’s not scare tactics. It’s science. And it’s happening right now in millions of homes across the U.S.
How Milk Thistle Actually Works in Your Liver
Milk thistle isn’t just another herbal trend. Its active ingredient, silymarin, is a mix of compounds like silybin, silychristin, and silydianin. These aren’t just antioxidants-they directly talk to your liver’s drug-processing system. That system? The cytochrome P450 enzymes, especially CYP3A4, CYP2C9, and CYP2D6. These enzymes break down about 70% of all prescription drugs you take. When milk thistle messes with them, it changes how fast or slow your meds get cleared from your body.Most supplements contain 70-80% standardized silymarin. Typical doses? 140 mg to 420 mg daily. That’s what most clinical trials used. But here’s the catch: not everyone responds the same way. Your genes, your diet, even your gut bacteria affect how silymarin behaves. One person might see zero effect. Another might end up with dangerously high levels of their blood thinner.
The Real Risk: Which Drugs Are Affected?
Not all drugs are equally at risk. The big red flags are medications with a narrow therapeutic index-meaning the difference between a helpful dose and a toxic one is tiny.- Warfarin (Coumadin): This blood thinner is metabolized by CYP2C9. Studies show milk thistle can inhibit this enzyme, leading to higher warfarin levels and increased bleeding risk. Real-world reports on Reddit and patient forums confirm this: people on stable warfarin doses saw their INR spike after starting milk thistle, forcing doctors to cut their warfarin by 15-35%.
- Phenytoin: Used for seizures, this drug also rides on CYP2C9. Even small changes in enzyme activity can cause seizures to return-or lead to dizziness, confusion, and loss of coordination.
- Statins: Drugs like atorvastatin and simvastatin are broken down by CYP3A4. While most clinical trials show no major interaction, some case reports suggest elevated muscle pain or liver enzyme spikes when combined with high-dose milk thistle. The risk is low, but it’s there.
- Immunosuppressants: Cyclosporine and tacrolimus, used after transplants, are highly sensitive to CYP3A4 changes. A slight increase in their levels can cause kidney damage. Doctors avoid milk thistle in transplant patients for this reason.
On the flip side, many drugs show no meaningful interaction. Direct-acting antivirals for hepatitis C-like sofosbuvir/velpatasvir-aren’t broken down by CYP enzymes in a way that milk thistle disrupts. Many patients take both without issue. Same goes for most antidepressants, thyroid meds, and insulin.
The Contradictory Science: Inhibits or Induces?
Here’s where it gets messy. Milk thistle doesn’t just block enzymes. It can also turn them on-but only after weeks of use.A 2020 study found that after just a few days, silymarin slightly blocked CYP2C9. But after 28 days of daily use, the same enzyme started working faster. That’s called enzyme induction. It means your body starts clearing drugs more quickly, which could make your meds less effective.
So if you start milk thistle and feel your blood pressure med isn’t working as well after two weeks, it might not be your condition worsening-it could be your liver suddenly processing it faster. This biphasic effect makes predicting outcomes nearly impossible without testing.
And that’s not all. Some studies show no effect at all. A 2019 trial gave 420 mg of silymarin daily to 24 healthy people for two weeks. They used midazolam-a classic CYP3A4 marker-and found only a 7.2% rise in drug levels. That’s below the 20% threshold experts consider clinically relevant. So why do some people have problems?
Answer: variability. Bioavailability of silybin is only 20-50%. Some supplements contain way less than labeled. A 2022 FDA review found only 32% of milk thistle products met their label claims. If you’re taking a weak product, you might get no effect. If you’re taking a potent one, you could be at risk.

How It Compares to Other Liver Supplements
Not all liver herbs are the same.- NAC (N-acetylcysteine): Great for detox and glutathione support. But it doesn’t touch CYP enzymes. If you want liver support without interaction risk, NAC is safer.
- Artichoke extract: Also inhibits CYP2C9-but more consistently. If you’re on warfarin, artichoke might be just as risky as milk thistle.
- Ursodeoxycholic acid: A pharmaceutical liver drug. It works differently, has predictable effects, and comes with clear dosing. But it’s expensive and can cause diarrhea. Milk thistle wins on safety, but loses on precision.
Milk thistle’s biggest advantage? Safety. Across 3,846 people in clinical trials, only 1.2% reported side effects-mostly mild stomach upset. Compare that to pharmaceutical options, where side effects hit 8.7%. For long-term use in fatty liver disease, milk thistle is often the go-to. But that doesn’t mean it’s risk-free when mixed with meds.
What Doctors Really Think
There’s a split in the medical community.Dr. Joseph Pizzorno, a leading integrative medicine expert, says the fear is overblown. He points to just 12 documented case reports in 40 years-and none proved causation. He argues that if milk thistle were truly dangerous, we’d see hundreds of ER visits.
But Dr. David S. Bernstein, a hepatologist at UConn, disagrees. He says: “We don’t have standardized extracts. We don’t know the exact dose that triggers interactions. And we can’t test every patient’s enzyme activity. So we err on the side of caution.”
That’s why guidelines differ. The European Medicines Agency says interactions are unlikely. The U.S. NIH’s LiverTox database says milk thistle is “possibly interacting” with CYP2C9 drugs. The FDA doesn’t require supplement labels to warn about drug interactions-so you won’t see it on the bottle.
What You Should Do (Practical Steps)
If you’re on any prescription drug and thinking about taking milk thistle-or already are-here’s what to do:- Check your meds. Are you on warfarin, phenytoin, cyclosporine, tacrolimus, or a statin? If yes, talk to your doctor before starting milk thistle.
- Don’t assume it’s safe. Just because it’s “natural” doesn’t mean it’s harmless. Natural doesn’t mean inert.
- Use standardized products. Look for “70-80% silymarin” on the label. Avoid vague claims like “pure milk thistle extract.”
- Monitor closely. If you’re on warfarin, get your INR checked weekly for the first month after starting milk thistle. For phenytoin, ask your doctor to check blood levels at days 3, 7, and 14.
- Track your symptoms. Unexplained bruising, dizziness, muscle pain, or fatigue after starting milk thistle? That’s a red flag.
- Wait 48 hours before lab tests. If your doctor wants to check drug levels, stop milk thistle for two days first. Otherwise, results could be skewed.
Bottom Line: It’s Not All Risk-But It’s Not All Safe Either
Milk thistle has real benefits. For people with fatty liver disease, it improves liver enzymes in over 65% of cases. It’s gentle, affordable, and widely tolerated. But if you’re on meds metabolized by the liver, it’s not a harmless add-on.Think of it like this: Milk thistle isn’t a vitamin. It’s a liver modulator. And your liver is the command center for your medications. Changing how it works-even slightly-can change how your drugs behave.
For most people not on critical meds, milk thistle is fine. For those who are? Talk to your doctor. Get tested. Don’t guess. Your liver might thank you. But your meds? They need clarity.
Can milk thistle raise my INR levels if I’m on warfarin?
Yes. Multiple case reports and user testimonials confirm that milk thistle can increase INR levels in people taking warfarin. This happens because silymarin inhibits the CYP2C9 enzyme, which breaks down warfarin. If you’re on warfarin and start milk thistle, get your INR checked weekly for the first month. You may need a dose adjustment.
Is milk thistle safe with statins?
Most clinical studies show no significant interaction between milk thistle and statins like atorvastatin or simvastatin. However, because statins are processed by CYP3A4-and milk thistle can affect this enzyme-there’s a theoretical risk. If you experience unexplained muscle pain or weakness after starting milk thistle, stop it and talk to your doctor.
How long does it take for milk thistle to affect liver enzymes?
Inhibition of liver enzymes like CYP2C9 can happen within 24-48 hours of starting milk thistle. But enzyme induction-where your liver starts breaking down drugs faster-takes 7-10 days of consistent use. This means effects can change over time, even if you don’t change your dose.
Are all milk thistle supplements the same?
No. Only 32% of milk thistle supplements tested in a 2022 FDA study met their label claims for silymarin content. Some contain far less than advertised, while others may be contaminated. Look for products that specify 70-80% standardized silymarin and are third-party tested (look for USP, NSF, or ConsumerLab seals).
Can I take milk thistle if I’ve had a liver transplant?
Generally, no. Transplant patients take immunosuppressants like cyclosporine or tacrolimus, which are highly sensitive to CYP3A4 changes. Even small changes in how these drugs are metabolized can lead to organ rejection or toxicity. Most transplant centers advise against milk thistle unless under strict medical supervision.
Does milk thistle help with fatty liver disease?
Yes. In over 65% of clinical studies, milk thistle improved liver enzyme levels (ALT, AST) in people with non-alcoholic fatty liver disease (NAFLD). It also reduced liver inflammation and fat buildup in some trials. It’s one of the few supplements with solid evidence for NAFLD-but it’s not a cure. Lifestyle changes remain the foundation of treatment.
What Comes Next?
The future of milk thistle is moving toward precision. Researchers are testing new formulations-like silybin bound to phosphatidylcholine-that improve absorption and reduce CYP interactions. Some companies are even exploring genetic testing to match doses to individual enzyme profiles.But until then, the rule is simple: If you’re on meds that your liver processes, don’t add milk thistle without talking to your doctor. And if you’re already taking it? Tell them. Bring the bottle. Ask: “Could this be affecting my other meds?”
Because when it comes to your liver and your pills, the quietest interactions are often the most dangerous.

Milk thistle's biphasic effect on CYP enzymes is underappreciated. Most people assume it's just an inhibitor, but the induction phase after 7-10 days is clinically significant. I've seen patients on phenytoin come in with breakthrough seizures after two weeks of 'natural liver support.' The delay makes it easy to miss.
This is so important. I'm a pharmacist and I see this all the time. People think 'natural' equals 'safe' and start popping milk thistle with their warfarin like it's a vitamin. Then they show up with INR 8.5 and bruising everywhere. The FDA doesn't require warnings on supplements, so the burden falls on us to educate. Please, if you're on meds, talk to your pharmacist before adding anything.
Also, third-party testing matters. I recommend only products with USP or NSF certification. The 2022 FDA review showing only 32% met label claims? That's terrifying. You could be taking a placebo or something way stronger than you think.
I'm sorry, but this whole article is just Big Pharma fear-mongering disguised as science. 🤡 Who even trusts the FDA anymore? They banned turmeric for years while approving toxic synthetic drugs. Milk thistle has been used for 2,000 years. Your liver knows what to do with it. Stop listening to doctors who get paid by drug companies. 🌿💚
The real issue isn't milk thistle-it's the pharmaceutical industry's failure to standardize drug metabolism testing. We're treating patients like lab rats with one-size-fits-all dosing while ignoring genetic variability in CYP enzymes. The science is clear: we need pharmacogenomic screening before prescribing anything metabolized by CYP3A4 or CYP2C9. Milk thistle is just the symptom, not the disease.
i been takin milk thistle with my atorvastatin for 8 months no problem. maybe its the brand i use? i got it from local ayurvedic shop. no side effects. maybe its just me?
One must contemplate the metaphysical duality of botanical intervention: is the liver a machine to be calibrated, or a sacred vessel to be honored? Milk thistle, in its quiet persistence, reminds us that nature does not operate on the linear timelines of pharmacokinetics. The enzyme induction observed after 28 days is not a flaw-it is a dialogue. We have forgotten how to listen to the body's whispers. We demand instant results, then blame the herb when the system responds in its own time.
Perhaps the true danger lies not in silymarin, but in our arrogance: believing we can quantify, control, and predict the rhythms of a living organism with clinical trials designed for synthetic molecules.
bro if you on statins and milk thistle and feelin muscle pain stop it now. i did and my creatine kinase went down in 3 days. dont be dumb. its not worth it. talk to your doc. your liver is tough but your muscles ain't.
As someone from India where herbal medicine is part of daily life, I've seen both sides. Many elderly take milk thistle with blood pressure meds without issue. But when my cousin started it with warfarin after reading a blog, her INR jumped from 2.3 to 4.8 in 10 days. We rushed to the hospital. The point isn't to fear herbs-it's to respect them. Always check. Always monitor. Knowledge is your best supplement.
Let me tell you what REALLY happened. I took milk thistle with my simvastatin for six months. Felt great. Then one morning I woke up and my left leg felt like it was wrapped in concrete. Couldn't lift my foot. ER doctor said rhabdo. My CPK was 18,000. They said it was probably the combo. I sued the supplement company. They said 'natural ingredients' on the label. Natural my ass. I lost my job because I couldn't walk for three months. Now I only take vitamins with 'FDA approved' stamped on them. And I don't trust anything that doesn't come in a pill with a barcode.
PS: My doctor said I'm lucky I didn't lose the leg. I'm lucky I didn't lose my life. And I'm still pissed.
This article is a masterpiece of corporate-sponsored FUD. You cite a 2019 trial with 24 people and call it 'no clinically relevant interaction'-but you ignore that 7.2% rise? That's a 1.5x increase in drug half-life. For warfarin, that's a 30% higher bleeding risk. And you call that 'minor'? Meanwhile, you dismiss case reports as 'anecdotal' while ignoring that real people die from these interactions every year. This isn't science-it's PR written by someone who gets kickbacks from Big Pharma.
This is the kind of info we need more of. So many people think supplements are harmless because they're 'natural.' But your liver doesn't care if something is plant-based or synthetic-it just sees a molecule. And if it interferes with your meds? That's dangerous. Thank you for laying it out clearly. I'm sharing this with my whole family.
I'm tired of this 'natural is better' nonsense. America has the best medical system in the world. If you're on prescription meds, take your meds. Don't go mixing in some hippie tea from a Walmart shelf. You think your great-grandma knew what CYP3A4 was? No. She didn't need to. She took her pills and lived. Stop playing scientist with your health.
What struck me most isn't the science-it's the silence. Why don't pharmacies warn people? Why don't doctors ask about supplements during med reviews? We'll ask about alcohol, smoking, even caffeine-but if someone says 'I take turmeric and milk thistle,' we nod and move on. That's not just negligence. It's a cultural blind spot. We treat pharmaceuticals as serious. We treat herbs as decoration.
The truth? Your liver doesn't care if the molecule came from a lab or a plant. It just wants to do its job. And if you're throwing in something that changes how it works? You're playing Russian roulette with your meds. Talk to someone who knows. Not a blog. Not a Reddit thread. A real clinician.
The FDA is in bed with Big Pharma. They don't want you to know that milk thistle is a natural CYP3A4 modulator because it would make billions in statin sales obsolete. They buried the 2018 NIH study showing silybin reduces cholesterol better than low-dose atorvastatin. They suppressed the 2021 trial where 80% of NAFLD patients reversed fatty liver with milk thistle + lifestyle. This is a cover-up. They're terrified of natural alternatives. Don't be fooled. 🕵️♀️💊 #MilkThistleIsTheTruth #BigPharmaLies