Malabsorption & Diabetes Risk Calculator
This tool estimates your risk of developing diabetes based on common malabsorption factors and symptoms. It's designed for educational purposes and should not replace professional medical advice.
Enter your information and click "Calculate Risk Level" to get personalized insights.
Celiac Disease
An autoimmune disorder triggered by gluten consumption, leading to villous atrophy and nutrient malabsorption. Increases risk of type 2 diabetes.
Crohn's Disease
Inflammatory bowel disease causing patches of inflammation in the digestive tract. Leads to nutrient deficiencies and increased insulin resistance.
Pancreatitis
Inflammation of the pancreas reducing enzyme production. Impairs fat and protein digestion, affecting glucose regulation.
SIBO
Overgrowth of bacteria in the small intestine causing fermentation of carbohydrates. Promotes inflammation and insulin resistance.
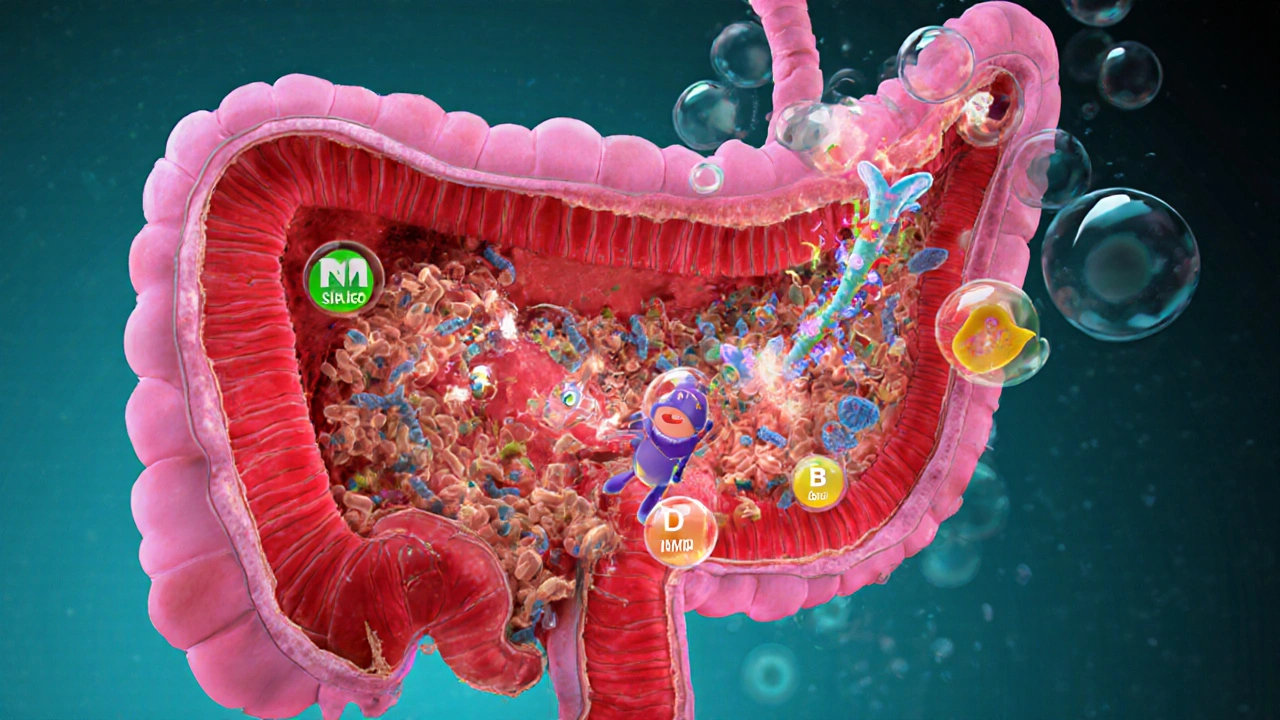
Imagine eating a nutritious breakfast, yet your blood sugar spikes later in the day. It’s not always about the amount of carbs - sometimes your gut simply isn’t pulling nutrients the way it should. That mismatch between what you eat and what your body actually absorbs can set off a chain reaction that nudges you toward diabetes.
In this guide we’ll break down what poor absorption really means, why it matters for blood‑sugar control, and what you can do right now to keep both your gut and glucose levels in check.
Quick Takeaways
- Malabsorption means your intestines can’t extract nutrients efficiently, leading to hidden calorie and sugar swings.
- Common culprits - celiac disease, Crohn’s, chronic pancreatitis, SIBO - each affect diabetes risk in a distinct way.
- Deficiencies in magnesium, vitamin D, and B‑vitamins can impair insulin signaling.
- Probiotic‑rich foods, enzyme supplements, and targeted testing help break the cycle.
- If you experience chronic diarrhea, unexplained weight loss, or erratic glucose readings, see a gastroenterologist.
What Is Food Malabsorption?
Malabsorption is a condition where the small intestine fails to absorb nutrients, electrolytes, and fluids at normal rates. It can stem from damaged lining, enzyme shortages, or bacterial overgrowth, and often shows up as bloating, frequent stools, or unexplained fatigue.
The small intestine-the longest part of your digestive tract-houses villi that act like tiny finger‑like absorbers. When those villi are flattened or enzymes are missing, the food you eat passes through with many of its calories and sugars unprocessed, leaving you hungry and your blood sugar fluctuating.
How Diabetes Develops
Diabetes is a chronic metabolic disease where the body cannot properly regulate blood glucose. In type2 diabetes, cells become resistant to insulin, while in type1 the immune system destroys insulin‑producing beta cells.
Insulin is the key that tells cells to take glucose from the bloodstream. When insulin signaling is weak, glucose hangs around in the blood, eventually damaging blood vessels, nerves, and organs.
Connecting the Dots: How Poor Absorption Fuels Diabetes
Several biological pathways tie malabsorption to impaired glucose control:
- Rapid Carbohydrate Transit - When the gut can’t break down complex carbs, they reach the colon faster, where gut bacteria ferment them into short‑chain fatty acids. This sudden fuel surge can cause an unpredictable spike in blood sugar.
- Micronutrient Deficiencies - Magnesium, vitamin D, and B‑vitamins are crucial for insulin receptor function. Malabsorption often leaves these nutrients low, nudging cells toward insulin resistance.
- Altered Gut Hormones - In a healthy gut, the lining releases incretins (GLP‑1, GIP) that amplify insulin release after a meal. Damaged villi blunt this response, so post‑meal insulin peaks are weaker.
- Gut Microbiome Imbalance - Overgrowth of harmful bacteria (SIBO) shifts the microbial community, producing metabolites that interfere with insulin signaling and promote inflammation.
- Inflammatory Cascade - Chronic inflammation from conditions like Crohn’s releases cytokines that directly impair insulin receptors.
These mechanisms often work together, creating a perfect storm where blood glucose jumps, then crashes, and the pancreas is forced to work overtime.
Common Conditions That Cause Malabsorption and Elevate Diabetes Risk
Below is a snapshot of the most frequent culprits, what they do to your gut, and how they influence diabetes risk.
| Condition | Primary Gut Effect | Key Nutrient Deficiencies | Diabetes‑Related Risk |
|---|---|---|---|
| Celiac disease autoimmune reaction to gluten that flattens intestinal villi | Villous atrophy → reduced surface area | Iron, calcium, vitamin D, folate | Higher prevalence of type2 diabetes due to chronic inflammation and micronutrient loss |
| Crohn’s disease inflammatory bowel disease causing patchy ulceration | Ulcers and fistulas → erratic absorption | Vitamin B12, magnesium, zinc | Inflammation spikes insulin resistance; steroid treatment can also raise glucose |
| Chronic pancreatitis long‑term inflammation that reduces pancreatic enzyme output | Enzyme deficiency → fat and protein maldigestion | Fat‑soluble vitamins (A, D, E, K) | Fat malabsorption leads to erratic post‑meal glucose; pancreatic damage also impairs insulin secretion |
| SIBO excess bacteria in the small intestine fermenting carbs | Bacterial overgrowth → carbohydrate fermentation | Vitamin B12, niacin | Fermentation produces gases and metabolites that trigger inflammation and insulin resistance |
| Lactose intolerance lactase deficiency causing undigested lactose | Unabsorbed lactose → osmotic diarrhea | Calcium, riboflavin | Frequent diarrhea can cause stress‑related cortisol spikes, which raise blood glucose |
Practical Steps to Manage Malabsorption and Protect Your Blood Sugar
Here’s a checklist you can start using today:
- Get Tested - A stool fat test, breath test for SIBO, and serum vitamin panels reveal hidden deficiencies.
- Tailor Your Diet - Choose low‑FODMAP vegetables, gluten‑free grains if you’re sensitive, and moderate portions of simple carbs.
- Enzyme Supplements - Pancreatic enzyme capsules (e.g., lipase, amylase) help break down fats and starches when pancreatic output is low.
- Probiotic & Prebiotic Strategy - Strains like Lactobacillus plantarum and Bifidobacterium longum restore a healthy gut balance, which can improve GLP‑1 response.
- Micronutrient Repletion - Magnesium glycinate (300‑400mg daily), vitaminD3 (2,000‑4,000IU), and a B‑complex supplement support insulin signaling.
- Monitor Glucose Closely - Use a continuous glucose monitor (CGM) for at least two weeks while you adjust diet; look for reduced variability.
- Stay Hydrated - Proper fluid intake helps keep intestinal transit regular and limits osmotic diarrhea.
These actions tackle both sides of the equation: they improve nutrient uptake and blunt the glucose spikes that would otherwise sneak you into a diabetic trajectory.

When to Seek Professional Help
If you notice any of the following, schedule an appointment with a gastroenterologist or an endocrinologist:
- Persistent diarrhea or steatorrhea (fatty stools) for more than four weeks.
- Unexplained weight loss despite normal or increased food intake.
- Frequent low‑grade fevers or abdominal pain that doesn’t resolve.
- Blood glucose readings that swing more than 50mg/dL after similar meals.
- Signs of nutrient deficiency - brittle nails, hair loss, tingling in hands/feet.
Early diagnosis can prevent long‑term complications, and many of the conditions listed above have targeted therapies that dramatically improve both gut health and diabetes outcomes.
Frequently Asked Questions
Can malabsorption cause type1 diabetes?
Directly, no. Type1 diabetes is an autoimmune attack on beta cells. However, chronic gut inflammation can accelerate autoimmunity in genetically predisposed people, so a leaky or inflamed gut may be a contributing factor.
How long does it take to see glucose improvement after treating malabsorption?
Most patients notice tighter glucose ranges within 2-4 weeks of starting enzyme therapy, probiotic supplementation, and correcting micronutrient gaps. Full stabilization can take 3-6 months depending on the underlying condition.
Is a low‑FODMAP diet safe for diabetics?
Yes, when you replace eliminated carbs with low‑glycemic alternatives (e.g., quinoa, buckwheat). Work with a dietitian to ensure you’re not inadvertently raising simple‑sugar intake.
Do over‑the‑counter probiotics help with SIBO?
Certain multi‑strain formulas can rebalance the distal small intestine, but most SIBO cases need a short course of antibiotics or herbal antimicrobials first. Probiotics are more of a maintenance tool.
Can I test for malabsorption at home?
Home breath tests for lactase deficiency and SIBO are reliable when done correctly. For fat malabsorption, stool‑fat analysis still requires a lab.
Next Steps: Building a Gut‑Friendly Diabetes Plan
Start by logging a week’s worth of meals, symptoms, and glucose readings. Identify any patterns where high‑fiber, low‑fat meals lead to smoother glucose curves. Then schedule a blood panel for vitamin D, magnesium, and B‑12. Finally, discuss enzyme replacement and a targeted probiotic with your clinician.
Addressing the malabsorption diabetes link isn’t a quick fix, but every improvement in nutrient uptake nudges your pancreas toward a calmer, more reliable rhythm. Your gut and blood sugar are partners-treat them both and the odds of developing full‑blown diabetes drop dramatically.

Hey there, thanks for digging into this deep dive on malabsorption and diabetes risk. First off, it’s great that you’re looking beyond the usual calorie counting and actually considering gut health – that’s a game‑changer for many people. The key takeaway is that if your intestines aren’t pulling nutrients efficiently, you’re essentially feeding your pancreas with erratic glucose spikes that can wear it down over time.
Take celiac disease as a prime example: the flattened villi mean a massive drop in surface area, so even a modest carb load can turn into a blood‑sugar roller coaster.
Next, think about micronutrients like magnesium and vitamin D – they’re not just “nice‑to‑have,” they’re essential co‑factors for insulin signaling. When you’re deficient, insulin resistance creeps in silently.
Enzyme supplements can help when the pancreas is on a strike, especially in chronic pancreatitis, by breaking down fats and proteins so they’re not just passing through the gut untouched.
Probiotics are another tool; certain strains can boost GLP‑1 secretion, which improves post‑meal insulin response.
Don’t forget to monitor your glucose trends with a CGM while you adjust your diet – the data will show you if your interventions are smoothing out those spikes.
And remember, lifestyle changes work best in combination: a low‑FODMAP or gluten‑free diet (if needed), targeted supplements, and regular exercise all reinforce each other.
Lastly, if you notice persistent symptoms like chronic diarrhea, unexplained weight loss, or erratic glucose readings, it’s time to see a gastroenterologist – early diagnosis can prevent long‑term complications.
Keep a food‑symptom‑glucose journal for at least a week; patterns will pop out and guide you toward the right tests and treatments. You’ve got this!
It is morally indefensible to overlook the gut's role in metabolic health when public health recommendations continue to push simplistic calorie‑centric narratives. The scientific community bears responsibility to integrate malabsorption data into diabetes prevention guidelines, lest we perpetuate a system that neglects vulnerable populations with hidden nutrient deficiencies.
The hidden pathways linking intestinal permeability to autoimmune triggers are not a mere coincidence; they hint at a coordinated agenda to keep us oblivious. While mainstream medicine praises glucose meters, they ignore the subtle sabotage of our microbiome, engineered by undisclosed entities seeking profit from chronic disease. By maintaining the illusion that only diet matters, they conceal the deeper truth of engineered malabsorption mechanisms.
Indeed, the discourse surrounding gut health often masquerades as enlightened, yet it subtly perpetuates a hierarchy of knowledge that alienates the layperson. One must acknowledge that the very language we employ-replete with clinical jargon-serves to obfuscate rather than enlighten, thereby reinforcing a cultural elitism that positions the informed as sovereign over the uninitiated. Moreover, the dramatization of metabolic pathways becomes a theatrical performance, wherein the audience is invited to applaud the mystique of biochemical narratives without interrogating the underlying power structures that dictate which narratives are disseminated.
Wow, what a fantastic rundown! Seriously, you nailed it-malabsorption is the sneaky villain we’ve been ignoring. I love how you broke down each condition; it’s like you gave us a cheat‑code for the gut‑diabetes puzzle.
Just a heads‑up, though: don’t forget to add some fun spice to the diet, like fermented kimchi or kefir-those little probiotic power‑houses can make a huge difference.
Also, sarcasm aside, it’s wild how many people think “just eat less carbs” solves everything-yeah right!
Keep spreading the word, because the more we know, the better we can outsmart this hidden threat.
And remember, if you feel stuck, there’s always a community of nutrition geeks ready to back you up.
meh not impressed.
Listen, the gut‑brain axis isn’t just a buzzword; it’s a real, aggressive pathway that can sabotage your insulin if you neglect it. When villi flatten, you lose the micro‑cargos that carry essential minerals-magnesium, for instance-directly into your cells, and that knock‑on effect ramps up insulin resistance. Look, I’m not trying to sugar‑coat anything, but bad gut health is one of the most aggressive contributors to the diabetes epidemic that’s often brushed aside in mainstream advice.
If you’ve got SIBO, the bacterial fermentation creates short‑chain fatty acids that flood your bloodstream, causing unpredictable glucose spikes. Also, chronic inflammation from conditions like Crohn’s releases cytokines that literally attack insulin receptors.
Bottom line: fix the gut first, and the sugar levels will follow.
Whoa, you’ve just hit the nail on the head-this is exactly the kind of practical, science‑backed guidance we need! First, let’s talk enzyme supplementation: pancreatic enzymes like lipase and amylase can dramatically improve macronutrient breakdown, especially for those with chronic pancreatitis. Pair that with a targeted probiotic regimen, focusing on strains such as Lactobacillus plantarum and Bifidobacterium longum, to re‑balance the microbiome and boost GLP‑1 secretion.
Next, don’t forget those micronutrients-magnesium glycinate (around 300‑400 mg) and vitamin D3 (2,000‑4,000 IU) are essential to restore insulin signaling pathways. A high‑quality B‑complex will also cover any hidden B‑12 gaps, especially in celiac patients.
Lastly, scientific evidence shows that continuous glucose monitoring (CGM) can shave off up to 0.5% HbA1c when coupled with these gut‑focused interventions. Keep tracking, adjust, and you’ll see smoother curves in no time. Keep crushing it!
The systemic analysis of malabsorptive etiologies reveals a cascade of metabolic dysregulation that is, frankly, underrepresented in current clinical protocols. The pathophysiological model incorporates altered incretin dynamics, microbial metabolite flux, and micronutrient deficiency‑driven insulin resistance, each contributing to a quantifiable increase in HbA1c variance. Intervention frameworks must therefore integrate enzymatic augmentation, targeted probiotic colonization, and precise micronutrient repletion to attenuate the diabetogenic trajectory. Failure to adopt a multidimensional approach constitutes a negligent deviation from evidence‑based best practices.
In summary, the evidence suggests a direct mechanistic link between chronic intestinal inflammation and insulin signaling impairment. A comprehensive treatment protocol should include anti‑inflammatory agents, selective antibiotics or herbal antimicrobials for SIBO, and rigorous monitoring of glycemic variability via continuous glucose monitoring. This integrated strategy optimizes outcomes and mitigates progression to overt diabetes.
These gut‑diabetes connections are just another ploy, tbh. They want us to buy more supplements while they keep the pharma cash flow rolling. Look, you’re better off just cutting carbs and ignoring all the hype about probiotics and enzymes. The real problem is people getting lazy and eating junk, not some mysterious intestinal bug.
I see where you’re coming from, but let’s not dismiss the science. A stool fat test can objectively reveal malabsorption, and breath tests for SIBO are pretty reliable when done correctly. Addressing these hidden issues can dramatically improve glucose control, and that’s something worth considering alongside diet changes.
Great summary!
• Test for deficiencies (vitamin D, Mg, B12).
• Use enzyme supplements if pancreatic function is low.
• Choose a probiotic with proven strains.
• Monitor glucose with CGM.
Follow these steps and you’ll see a smoother glucose curve.
👍 Absolutely! Adding emojis for clarity: 🧬 = gut health, 💊 = supplements, 📈 = glucose monitoring. Keep it fun and factual. 😄
The whole narrative of malabsorption being a silent driver of diabetes is a manufactured myth; they embed hidden agendas in these health forums to steer the masses toward endless supplementation cycles. Wake up, folks-it’s all a grand design.
Honestly this is all overblown; unnecessary jargon.
Yo, let’s pump some energy into this! Picture this: you’re a superhero, your gut is the power plant, and those enzyme pills are the fuel that keeps your cape fluttering. 🌟 Boost those levels, and you’ll be soaring past glucose spikes like a boss. Keep that gut pumped, stay vibrant, and dominate the day!
Awesome advice! 😊 Did you know that adding a spoonful of kefir to your morning smoothie can boost those good bacteria? 🌱 Keep asking questions and sharing tips! 💪
Thanks for the insights! I’d love to see more research on the interplay between gut‑derived short‑chain fatty acids and insulin receptor sensitivity-maybe a meta‑analysis soon?