When your kidneys start leaking protein, it’s not just a lab result-it’s your body screaming for help. For people with diabetes, albuminuria is that early warning sign most miss. It’s not a disease itself, but it’s the clearest signal that diabetic kidney disease (DKD) is already taking root. And here’s the hard truth: if you don’t catch it early, you’re on a path toward dialysis, heart attack, or early death.
What Albuminuria Really Means
Albumin is a protein your healthy kidneys keep in your blood. When they start to fail, albumin slips into your urine. That’s albuminuria. It’s not something you feel. No swelling, no pain, no symptoms-just a silent leak. That’s why testing is everything.
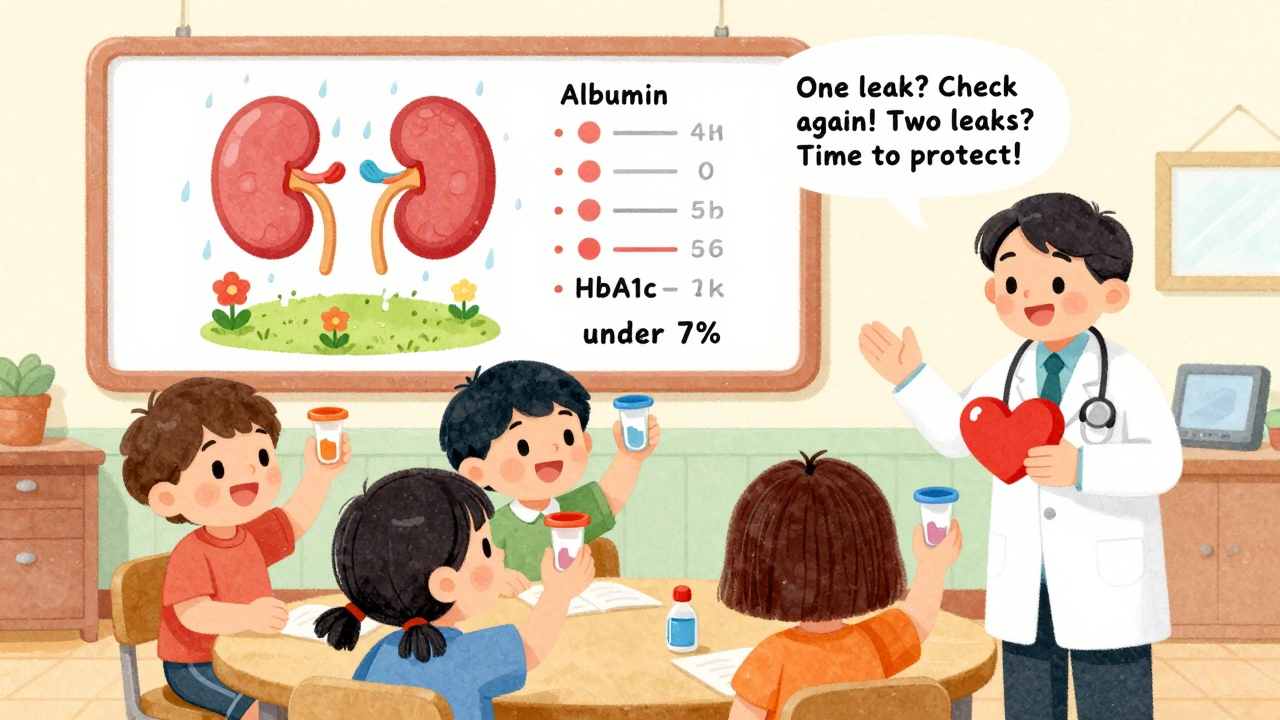
The standard test is the urine albumin-to-creatinine ratio, or UACR. Normal is under 30 mg/g. Anything above that? That’s kidney damage. The old terms-microalbuminuria and macroalbuminuria-are gone. Why? Because even a little albumin matters. KDIGO guidelines updated this in 2012, and now every major medical group agrees: any albumin in your urine means your kidneys are under stress.
But here’s the catch: one high reading doesn’t mean you have DKD. UACR can spike from a hard workout, a fever, or even your period. That’s why doctors need two out of three abnormal tests over 3 to 6 months to confirm it. Skipping retesting is like ignoring a smoke alarm because it went off once.
Why Albuminuria Is the Best Predictor of Disaster
Albuminuria isn’t just a marker-it’s a forecast. A 2021 study of over 128,000 people with diabetes found that those with UACR above 300 mg/g had a 73% higher risk of dying from any cause and an 81% higher risk of dying from heart disease than those with normal levels.
And it gets worse. Once albuminuria climbs into the severely increased range, your kidneys are racing downhill. The DCCT/EDIC trial showed that people with type 1 diabetes who kept their HbA1c under 7% cut their risk of developing albuminuria by nearly 40%. That’s not a small win. That’s a life saved.
For type 2 diabetes, the UKPDS study found that every 1% drop in HbA1c meant a 21% lower chance of kidney damage. That’s the power of tight control. It’s not about perfection. It’s about progress.

Tight Control Isn’t Just About Blood Sugar
Many think managing diabetes means watching carbs and taking insulin. But for your kidneys, it’s a three-part fight: blood sugar, blood pressure, and meds.
Most guidelines say your blood pressure should be under 140/90. But KDIGO says if your UACR is above 300 mg/g, aim for under 120/80. That’s aggressive. And it works. The SPRINT trial showed intensive blood pressure control cut macroalbuminuria by 39%. But here’s the trade-off: for every 47 people treated this way, one had a sudden kidney injury. That’s why most doctors stick with 140/90 unless you’re at high risk.
Medications are where things get powerful. ACE inhibitors and ARBs-like lisinopril or losartan-were the first line of defense. The IRMA-2 trial proved that losartan at 100 mg/day cut progression from micro- to macroalbuminuria by over half. And you don’t need high blood pressure to benefit. These drugs work directly on kidney filters.
Now, there’s a new player: SGLT2 inhibitors. Drugs like empagliflozin don’t just lower blood sugar-they protect kidneys. The EMPA-KIDNEY trial showed they reduced the risk of kidney failure by 28% in people with UACR over 200 mg/g. That’s huge. And they’re now recommended as first-line therapy, even if you don’t have high blood sugar.
Then there’s finerenone, a newer drug that blocks a harmful hormone in the kidneys. A 2024 study showed it cut albuminuria by 32% in just four months and slowed kidney decline by 23% over three years. It’s not for everyone-but for those already on an ACE or ARB, it’s a game-changer.
The Real Problem: No One’s Getting Tested
Here’s the broken part: we have the tools. We know what works. But most people never get tested.
NHANES data from 2017-2018 found that only 52.5% of U.S. adults with diabetes hit their HbA1c goal. Just 56.9% control their blood pressure. And only 12.2% nail all three: sugar, pressure, and cholesterol.
And screening? Only 58-65% of clinics even check UACR yearly, despite the American Diabetes Association calling it a Class A recommendation-the highest level of evidence. Why? Doctors don’t get reminders. Patients forget to bring samples. Labs don’t flag abnormal results.
One clinic in Boston started using EHR alerts that pop up every time a diabetic patient walks in. They added point-of-care urine tests so results come back in 10 minutes. They hired pharmacists to adjust meds. Within a year, UACR testing jumped from 61% to 92%. And the number of patients reaching UACR under 300 mg/g rose by 41%.
What You Can Do Right Now
If you have diabetes, here’s your action plan:
- Get your UACR tested every year. If you’re over 30, start now-even if you feel fine.
- If your UACR is above 30, get two more tests within six months. Don’t ignore it.
- Aim for HbA1c under 7%. If you’re young and healthy, ask about 6.5%.
- Keep your blood pressure under 140/90. If you have high albuminuria, push for 120/80 with your doctor.
- Ask if you’re on an ACE inhibitor or ARB. If not, ask why. If you are, ask if the dose is maxed out.
- Ask about SGLT2 inhibitors like empagliflozin or finerenone. These aren’t just for blood sugar-they’re kidney shields.
Don’t wait for swelling in your legs or fatigue. By then, it’s too late. Albuminuria is your early signal. Treat it like the emergency it is.
Why This Matters Beyond the Lab
Diabetic kidney disease doesn’t just hurt your kidneys. It kills your heart. It drains your bank account. The Chronic Renal Insufficiency Cohort study found that only 28.7% of people with DKD get all the recommended treatments. And the biggest reason? Money. Access. Fear.
But here’s the hope: if every diabetic patient got screened, treated, and followed up, we could prevent 1.2 million new cases of DKD in the U.S. by 2030. That’s 37% fewer people on dialysis. And $14.8 billion saved in healthcare costs.
This isn’t about perfect numbers. It’s about catching the leak before it becomes a flood. It’s about taking control before your kidneys give out. And it’s about knowing that the next step isn’t just another pill-it’s a second chance.
What is albuminuria and why does it matter in diabetes?
Albuminuria means protein (specifically albumin) is leaking into your urine, which signals kidney damage. In diabetes, it’s the earliest and most reliable sign of diabetic kidney disease (DKD). Even small amounts matter-anything above 30 mg/g on a UACR test indicates damage is starting. Left unchecked, it leads to kidney failure, heart disease, and early death.
How is albuminuria tested, and how often should I get checked?
It’s tested with a simple urine sample, measured as the urine albumin-to-creatinine ratio (UACR). A spot urine test is standard. You should be tested annually if you have type 2 diabetes (at diagnosis) or type 1 diabetes (after 5 years). If your result is abnormal, you’ll need two more tests within 3-6 months to confirm. Don’t rely on one high reading-it can be caused by infection, exercise, or high blood sugar.
Can tight blood sugar control really prevent kidney damage?
Yes. The DCCT/EDIC study showed that keeping HbA1c under 7% reduced new albuminuria by 39% in type 1 diabetes. For type 2, each 1% drop in HbA1c lowered DKD risk by 21%. The benefits last for decades-even if your control slips later. This is called "metabolic memory." It’s why early, tight control matters more than you think.
What medications protect the kidneys in diabetic kidney disease?
Three classes are proven: ACE inhibitors or ARBs (like lisinopril or losartan), SGLT2 inhibitors (like empagliflozin), and finerenone. ACE/ARBs reduce protein leakage and lower blood pressure. SGLT2 inhibitors protect kidneys independently of blood sugar control. Finerenone, a newer drug, reduces albuminuria and slows kidney decline even when used with ACE/ARBs. All three are now recommended together for high-risk patients.
Why aren’t more people getting tested or treated for albuminuria?
Three big reasons: clinics often lack EHR alerts to remind doctors to test, patients forget or skip urine collection (23% fail to return samples), and many providers don’t realize how critical albuminuria is as a predictor. Only 12.2% of U.S. adults with diabetes meet all three targets: blood sugar, blood pressure, and cholesterol. Systemic gaps in care, not lack of knowledge, are the real barrier.
Is it too late to help my kidneys if I already have albuminuria?
No. Reducing albuminuria-even by 30% from its peak-cuts your risk of kidney failure by nearly half. Studies show that bringing UACR below 300 mg/g or lowering it significantly slows disease progression and reduces heart attacks. Starting ACE inhibitors, SGLT2 inhibitors, or finerenone can reverse early damage. The goal isn’t perfection-it’s progress. Every step down from high albuminuria saves kidney function.

Albuminuria isn't just a lab anomaly-it's the first whisper of systemic failure in diabetic patients. The fact that we've moved away from 'micro' and 'macro' classifications is long overdue. Any detectable albumin means glomerular damage is underway, and we've spent too long treating it as a borderline issue. The data is clear: early intervention with ACE/ARBs and SGLT2 inhibitors alters trajectories. This isn't speculation-it's evidence-based medicine at its most actionable.
Yet, the real tragedy isn't the science-it's the system. Clinics don't prioritize UACR because it's not reimbursed well, and patients don't follow up because they're told 'you're fine' despite abnormal results. We need automated alerts, not reminders. We need pharmacists embedded in primary care, not afterthoughts.
And let's stop pretending that 'tight control' is just about HbA1c. It's the trifecta: glucose, BP, lipids. Only 12% hit all three? That's not patient failure. That's healthcare system failure.
Finerenone is the quiet revolution. It doesn't just lower albumin-it reprograms renal inflammation. We're talking about modifying disease progression, not just managing symptoms. And it works even when ACE/ARBs are already maxed out. Why isn't this first-line everywhere?
Let's not romanticize 'progress.' Progress is when UACR drops from 800 to 200. Not when someone 'tries harder' with carbs. This is pathophysiology, not willpower.
Really appreciate this breakdown. I’ve seen too many patients dismissed because their A1c is 'only' 7.8%-but if their UACR is 400, they’re already in danger. It’s not about being perfect, it’s about being proactive.
One thing I’ve noticed in Ireland: GPs are starting to use point-of-care dipsticks now. Not as accurate as lab tests, but it gets the conversation started. If a patient sees protein in their urine right then and there, they actually listen. It’s a small thing, but it changes engagement.
Also, SGLT2 inhibitors aren’t just for diabetes anymore. I’ve got a heart failure patient on empagliflozin who’s got no diabetes at all. Kidneys don’t care about your glucose-they care about pressure, inflammation, and filtration. This is a renal drug, first and foremost.
Oh wow. A post that doesn’t start with ‘eat less sugar’ and actually talks about real medicine? What is this, 2024?
Let me guess-the next comment will be someone saying ‘just drink more water’ and ‘avoid processed carbs.’
Meanwhile, the real solution? A pill that blocks a hormone your kidneys don’t even know they have, and it cuts albuminuria by a third in four months. And we’re still debating whether to test people annually?
It’s not that people don’t care. It’s that the system rewards inertia. Testing costs money. Medications cost more. And nobody gets a bonus for preventing dialysis five years from now.
So we wait until legs swell. Until they’re on the transplant list. Until the ER visit costs $50k. Then we’re ‘surprised.’
Pathetic. And predictable.
OMG I just cried reading this. I’m a type 2 diabetic for 12 years and I never knew albuminuria was a thing until my mom passed from kidney failure last year. She never had swelling, never complained-just got tired. They told her it was ‘aging.’
Now I test every single month. I’m on losartan, empagliflozin, and I walk 10k steps daily. My UACR dropped from 410 to 187 in 6 months. I’m not ‘cured’-but I’m fighting.
To anyone reading this: don’t wait for a funeral to wake up. Your kidneys don’t scream. They whisper. And if you don’t listen? They just… stop.
It is profoundly disconcerting to observe the persistent underutilization of evidence-based renal protective strategies within contemporary primary care paradigms. The convergence of clinical guidelines from KDIGO, ADA, and ESC is unequivocal: early detection of albuminuria, coupled with pharmacologic intervention via RAAS blockade and SGLT2 inhibition, constitutes a paradigm shift in the management of diabetic kidney disease.
Moreover, the metabolic memory phenomenon, as elucidated by the DCCT/EDIC cohort, underscores the imperative of early glycemic control-not merely as a therapeutic objective, but as a prophylactic intervention with lifelong ramifications. The economic burden of end-stage renal disease, estimated at $48 billion annually in the United States, is not merely a fiscal concern-it is a moral indictment of a fragmented healthcare infrastructure that prioritizes acute intervention over chronic prevention.
One must question the sociopolitical determinants that inhibit the widespread implementation of point-of-care UACR testing, particularly in underserved communities where disparities in screening frequency are most pronounced. The solution is not merely clinical; it is systemic, structural, and ethically non-negotiable.
Y’all are overcomplicating this. I’ve got type 2, my UACR was 500, I started empagliflozin + losartan, cut soda, walked 30 mins a day, and now it’s 140. No magic. No miracle. Just consistency. 💪
And yes, finerenone? I’m on it now too. My doc said it’s expensive but insurance covered it after I begged. If you’re over 30 with diabetes, you owe it to yourself to ask for these meds. Don’t wait for your legs to puff up like balloons. I saw a guy on dialysis last week-he was 41. Bro, you had 10 years to act.
Also, stop blaming the patient. If your doctor doesn’t mention UACR at your annual visit, fire them. Find someone who cares. Your kidneys don’t care if you’re ‘busy.’ They’re just trying to keep you alive.
Wow. Someone actually wrote a post that’s 90% accurate and doesn’t end with ‘eat more kale.’
Still, the whole ‘tight control saves kidneys’ thing is overstated. I’ve seen people with HbA1c 5.8% and UACR 1200 because their BP was 160/100 and they were on metformin only. Sugar isn’t the villain. Hypertension is.
Also, SGLT2 inhibitors cause yeast infections. Like, a lot. So if you’re a woman, good luck with that. And finerenone? It raises potassium. So now you need to get blood tests every week. Great.
This isn’t a superhero story. It’s a lifelong medical treadmill. And most people just want to live without 7 pills and 3 lab draws a month.
Man, I wish my doc talked like this. I got diagnosed with type 2 last year and all I heard was ‘watch your carbs.’
Turns out, I needed a urine test I didn’t even know existed. My UACR was 380. Scared the crap outta me.
Now I’m on losartan and Jardiance. My BP’s down, my energy’s up. I still eat pizza, but I test my urine every month now. It’s not perfect, but it’s better.
Thanks for the straight talk. 👍
How can you trust Western medicine when they ignore Ayurveda? In India, we’ve been treating diabetic nephropathy with Gokshura, Punarnava, and Triphala for 5,000 years. No drugs. No side effects.
These SGLT2 inhibitors? They’re just patented Western chemicals. You think your kidneys don’t know the difference? They’re foreign to your body.
And why do you think only 12% hit all targets? Because you’re overmedicating. Your body isn’t a machine to be fixed with pills. It’s a temple. You need balance, not biochemistry.
Also, why is everyone talking about ‘albuminuria’ like it’s some new discovery? Our grandmothers knew kidney damage started with foamy urine. We just forgot.
Bro this is gold. I’m from India, type 2 for 8 years. My uncle died on dialysis. I didn’t know anything until I read this.
I got my UACR tested last month-was 210. Started empagliflozin and walked 10k steps every day. My doc didn’t even mention it before. Just gave me metformin and said ‘eat less rice.’
Now I’m telling everyone in my family to get tested. My sister got hers done and hers was 80. She’s fine now. But if she waited? Who knows.
Also, finerenone? Sounds expensive but I’m asking my doctor. If it saves kidneys, it’s worth it. No point living if your body’s falling apart.
I’ve been a nurse for 22 years and I’ve watched too many people lose their kidneys because no one ever said ‘let’s check your urine.’
One patient, 54, diabetic since 22, never had symptoms. Came in for a foot sore. We tested UACR-was 980. He cried. Said he thought he was doing fine because he didn’t feel sick.
He’s on dialysis now. But he’s alive. Because we caught it late, not too late.
Don’t wait to feel bad. Your kidneys don’t have a volume button. They don’t scream. They just… go quiet.
Test. Talk. Treat. Don’t let fear silence you.
Let’s be real-this whole albuminuria obsession is a Big Pharma fantasy. ACE inhibitors? ARBs? SGLT2 inhibitors? All patented drugs with massive profit margins. And now finerenone? Another billion-dollar pill.
Meanwhile, the real cause of diabetic kidney disease? Chronic inflammation from ultra-processed foods. The real solution? Whole foods, fasting, and stress reduction. Not chemicals.
And why is everyone ignoring the fact that 70% of diabetics in developing nations can’t even afford insulin, let alone a $1,200/month kidney drug?
This isn’t medicine. It’s a market segmentation strategy disguised as science. The real tragedy? People believe it.
I appreciate the depth here. As someone who works in public health, I’ve seen clinics where the EHR doesn’t even have a checkbox for UACR testing. It’s not that providers are negligent-it’s that the system doesn’t make it easy.
What we need isn’t more awareness campaigns. We need embedded protocols. A simple algorithm: If patient has diabetes → auto-generate UACR order → send reminder to patient → auto-flag if abnormal → trigger pharmacist consult.
It’s not rocket science. It’s workflow design.
And yes, finerenone is expensive-but so is a kidney transplant. We’re paying either way. The question is: who pays? The patient? Or the system?
Great post but typos: ‘UACR’ not ‘UACR’ in second paragraph. And ‘empagliflozin’ misspelled as ‘emagliflozin’ in one place. But the info is solid.
My dad’s UACR was 420 last year. Started on losartan. Now it’s 160. He’s 72. Still walks 2 miles every morning. Says he feels better than he has in 10 years.
Don’t wait. Test. Talk. Take the pill. Your future self will thank you.
Interesting point about finerenone’s cost. But here’s the math: in the FIDELIO-DKD trial, for every 14 patients treated with finerenone over 3 years, one avoided kidney failure or cardiovascular death. That’s a 7% absolute risk reduction.
At $1,200/month, that’s $43,200 per patient over three years. Dialysis? $90,000/year. Transplant? $300,000 upfront. Insurance companies know this. That’s why they’re covering it now.
It’s not a drug. It’s an investment. And the ROI isn’t just financial-it’s human.
Also, correction: I didn’t say ‘metabolic memory’ was the only reason early control matters. I said it’s one of the most profound. The damage reversal from early intervention? That’s the real miracle. Not the drug. The timing.