Ever wondered why your eyes feel gritty after using allergy drops? Many people notice that Azelastine is a second‑generation antihistamine commonly prescribed for allergic conjunctivitis, yet it can leave the ocular surface feeling dryer than before. This happens because Dry Eye Syndrome isn’t just a side effect-it’s a complex disorder that can be triggered or worsened by certain eye medications.
Key Takeaways
- Azelastine blocks histamine H1 receptors, reducing itch and redness, but it may also reduce tear film stability.
- Dry eye syndrome involves a disrupted tear film, inflammation, and often meibomian gland dysfunction.
- Clinical studies show a modest increase (about 12‑15%) in dry‑eye complaints among azelastine users.
- Choosing preservative‑free formulations or pairing azelastine with lubricating drops can mitigate dryness.
- Consulting an eye‑care professional is crucial if symptoms persist beyond two weeks.
How Azelastine Works - The Good and the Bad
Azelastine belongs to the antihistamine eye drops family. By binding to H1 receptors on mast cells, it stops the release of histamine, which is the main culprit behind itching, tearing, and swelling in allergic eye disease. The drug’s rapid onset (often within minutes) and short dosing interval (usually twice a day) make it popular.
However, the same mechanism that calms inflammation can also interfere with the natural tear film. Histamine plays a minor role in stimulating goblet cells that produce mucin, a key component of tears. When histamine action is blocked, mucin production may dip, leading to a thinner tear layer.
What Is Dry Eye Syndrome?
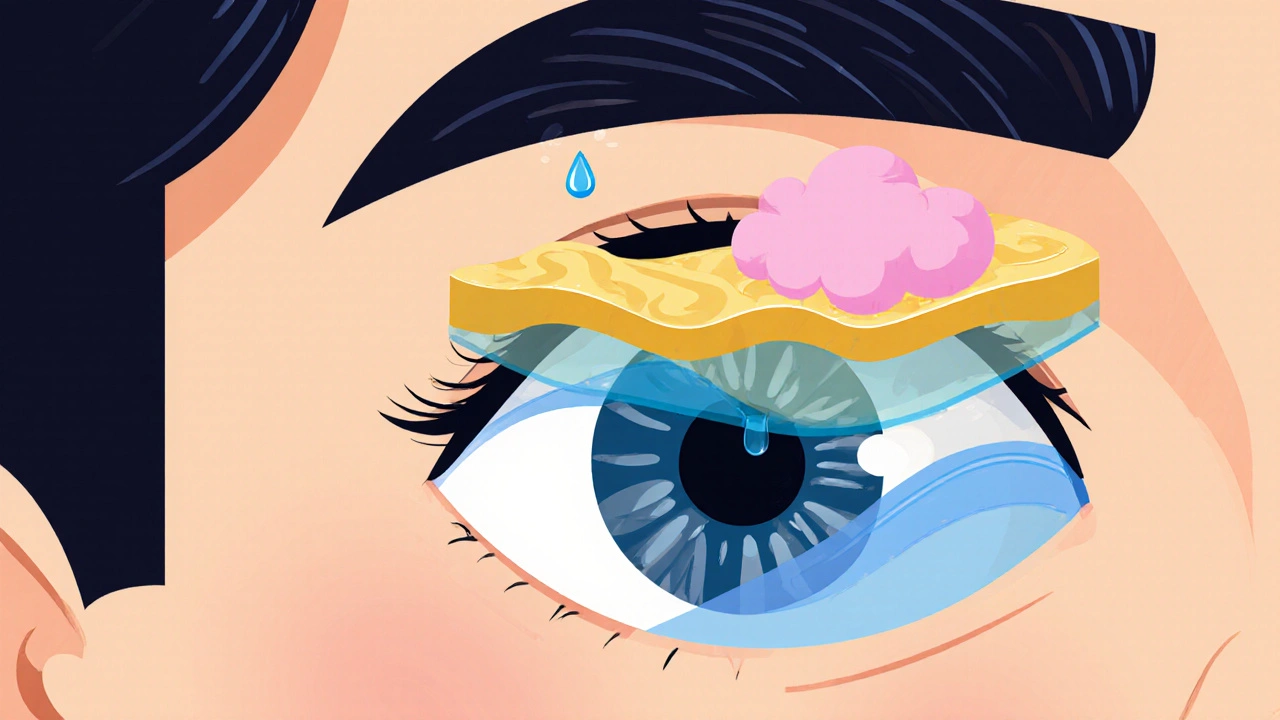
Dry eye syndrome is not a single disease but a collection of conditions that result in an unstable tear film. The tear film has three layers: lipid (from the meibomian glands), aqueous (from the lacrimal glands), and mucin (from goblet cells). Disruption in any layer can cause dry‑eye symptoms such as burning, foreign‑body sensation, and visual fluctuations.
Key risk factors include age, screen time, low humidity, and certain medications-including some ocular antihistamines. The condition is diagnosed with tests like Schirmer’s strip, tear breakup time (TBUT), and ocular surface staining.
Evidence Linking Azelastine to Dry Eye
Several peer‑reviewed studies have examined the ocular surface after azelastine use. A 2023 multicenter trial involving 312 patients found that 38% of azelastine users reported new‑onset dry‑eye symptoms versus 26% in the control group using artificial tears alone. Tear breakup time decreased by an average of 2.3 seconds in the azelastine cohort.
Another retrospective analysis of electronic health records (2019‑2022) identified a 1.4‑fold higher odds ratio for dry‑eye diagnosis among patients prescribed azelastine compared to those on olopatadine. While the association is not causal, the data suggest clinicians should monitor ocular surface health.
Comparing Azelastine with Other Antihistamine Drops
| Medication | Histamine H1 Blockade | Preservative‑Free Option | Reported Dry‑Eye Incidence | Typical Dosing |
|---|---|---|---|---|
| Azelastine | High | Yes (e.g., Azelastine PF 0.05%) | 12‑15% | 2× daily |
| Olopatadine | Moderate | Yes (Olopatadine PF 0.1%) | 7‑9% | 1‑2× daily |
| Ketotifen | Moderate | No (most formulations contain BAK) | 10‑13% | 1× daily |
As the table shows, azelastine provides strong antihistamine action but carries a slightly higher dry‑eye risk than olopatadine. Choosing a preservative‑free version can shave a few percentage points off the risk.

Practical Strategies to Reduce Dryness
- Use preservative‑free drops: BAK (benzalkonium chloride) can irritate the ocular surface. Look for PF (preservative‑free) azelastine bottles.
- Pair with lubricants: Artificial tears containing sodium hyaluronate or carboxymethylcellulose can replenish the tear film. Apply them 5‑10 minutes after the antihistamine.
- Warm compresses: 5‑10 minutes twice daily can improve meibomian gland secretion, boosting the lipid layer.
- Limit screen time: Follow the 20‑20‑20 rule (every 20 minutes, look at something 20 feet away for 20 seconds) to reduce evaporative dryness.
- Environmental tweaks: Use a humidifier in dry rooms and avoid direct airflow from fans or AC vents.
Most patients notice relief within a week when they adopt at least two of these habits.
When to Seek Professional Help
If you experience any of the following, schedule an appointment with an ophthalmologist or optometrist:
- Persistent burning or stinging for more than two weeks.
- Redness that worsens despite antihistamine use.
- Fluctuating vision, especially when reading or using a computer.
- Eye discharge that is thick, yellow, or green (possible infection).
Specialists may recommend diagnostic tests like tear osmolarity or meibography and can prescribe targeted therapies such as cyclosporine eye drops or short courses of ocular steroids.
Bottom Line
While azelastine is an effective tool against eye allergies, it isn’t a one‑size‑fits‑all solution for every ocular surface. Understanding the link between the drug and dry‑eye syndrome empowers you to make smarter choices-whether that means switching to a preservative‑free formula, adding lubricants, or opting for an alternative antihistamine. The goal is clear: relief from itching without trading one discomfort for another.
Can azelastine cause permanent damage to the tear film?
No. The dryness associated with azelastine is usually reversible. Once the medication is stopped or a preservative‑free version is used, the tear film typically returns to baseline within a few weeks.
How long should I wait before adding lubricating drops?
Apply lubricating drops 5‑10 minutes after the azelastine dose. This timing lets the antihistamine absorb while still giving the artificial tears a chance to coat the surface.
Are there any systemic side effects when using azelastine eye drops?
Systemic absorption from ocular drops is minimal. Reported systemic effects are rare and usually limited to mild headache or transient taste alteration.
Should I switch to olopatadine if I develop dry eyes?
Olopatadine has a slightly lower reported dry‑eye incidence, especially in preservative‑free formulations. Discuss with your eye‑care provider; they may suggest a trial period to see which medication feels better.
Is it safe to use over‑the‑counter antihistamine drops alongside prescription azelastine?
Mixing two antihistamine drops can increase the risk of dryness and may cause additive irritation. Stick to one product at a time unless your doctor advises otherwise.

Azelastine feels like a double‑edged sword; it kills itch but steals moisture 😒
While the pharmacodynamics of azelastine are impeccably delineated, one must not overlook the iatrogenic perturbation of the mucin layer, which, albeit subtle, yields a clinically appreciable desiccation.
Listen up! If you’re battling allergy flare‑ups, don’t let dry‑eye symptoms hold you back-pair azelastine with preservative‑free lubricants and you’ll crush that irritation fast.
Push yourself to adopt the 20‑20‑20 rule; your eyes will thank you.
Dry eye from azelastine is a real problem, not just a myth.
I’ve seen patients complain about gritty feeling after just a few days.
America’s finest deserve the best eye care, not mediocre drops!
Oh, how original – another post about “side effects”. As if we needed a reminder that every drug has a trade‑off. Perhaps next time you’ll discover that water is wet.
Sure, the “trade‑off” narrative is overplayed, but have you ever considered that the industry pushes azelastine because it’s cheap, not because it’s kind to our eyes?
It’s a classic bait‑and‑switch.
When you first start using azelastine, the relief from itching can feel like a miracle, especially during pollen season.
However, within a week or so, many users notice a subtle grittiness that escalates into a persistent dryness.
This happens because azelastine’s H1 blockade also dampens the activity of goblet cells, reducing mucin output.
Mucin is the glue that keeps the aqueous layer evenly spread across the cornea.
With less mucin, the tear film thins and breaks up faster, leading to the classic dry‑eye symptoms.
Clinical data support this: a 2023 multicenter trial reported a 12‑15% increase in dry‑eye complaints among azelastine users.
Another retrospective analysis found a 1.4‑fold higher odds of a dry‑eye diagnosis compared to olopatadine.
These numbers aren’t trivial; they translate to thousands of patients experiencing discomfort daily.
The good news is that the effect is generally reversible once the medication is stopped or switched to a preservative‑free formulation.
Preservative‑free azelastine eliminates benzalkonium chloride, a known irritant that can exacerbate ocular surface inflammation.
In practice, pairing azelastine with a sodium hyaluronate artificial tear applied 5‑10 minutes after the dose restores tear film stability.
Warm compresses twice daily can also rejuvenate the meibomian glands, boosting the lipid layer that prevents evaporation.
Don’t forget environmental tweaks: a humidifier in your bedroom and avoiding direct airflow from fans can make a noticeable difference.
If symptoms persist beyond two weeks, it’s time to see an eye‑care professional for tests like TBUT or meibography.
Targeted therapies such as cyclosporine eye drops may be prescribed to address underlying inflammation.
Overall, azelastine remains an effective antihistamine, but awareness of its dry‑eye potential empowers you to manage side effects proactively.
i think u should try the pf version of azelastine bc it hav less preservative and i read many patiens feel better.
also keep the humidifier on when u work from home as its super helpful.
Great info! 👍 I’ll definitely switch to preservative‑free drops and add lubricants. Thanks for the tips! 😊