Opioid Tapering Calculator
Understanding Physical Dependence vs. Addiction
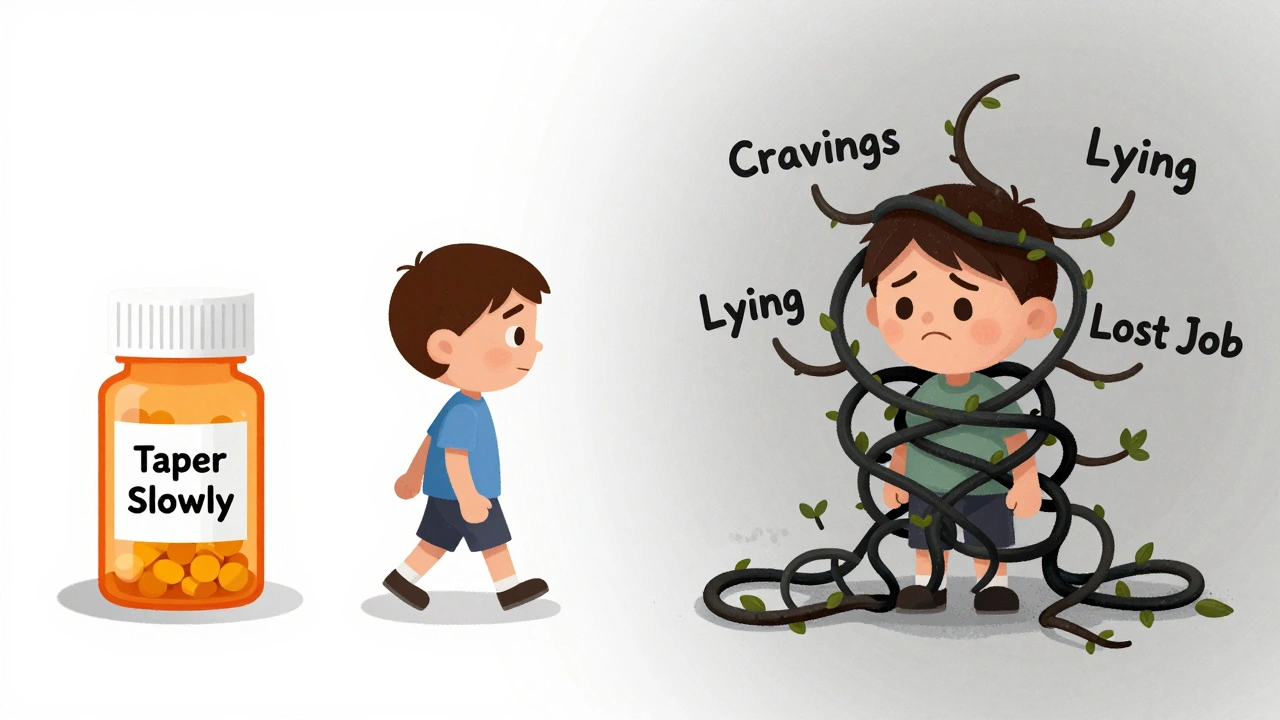
This calculator helps you create a safe tapering plan if you're physically dependent on opioids but not addicted. Remember: Physical dependence is a normal biological response to opioids, not addiction. Addiction (Opioid Use Disorder) involves loss of control, compulsive use despite harm, and intense cravings.
Calculate Your Safe Tapering Schedule
Your Tapering Schedule
Initial Dose: MME
Reduction Rate:
Estimated Duration:
Final Dose: MME
Frequency: Every
Medical Supervision Needed:
Your Tapering Steps:
Important Safety Notes
The CDC recommends that all opioid tapers be done under medical supervision, especially if you have been taking high doses or have certain health conditions. If you experience severe withdrawal symptoms (e.g., intense nausea, vomiting, seizures), contact your doctor immediately.
Many people think if you take opioids for a while and then feel sick when you stop, you’re addicted. That’s not true. You might just be physically dependent. And confusing the two can cost people their pain relief, their dignity, or even their lives.
What Physical Dependence Really Means
Physical dependence is your body getting used to having a drug in your system. It’s not a choice. It’s biology. If you take opioids - whether it’s oxycodone for a broken bone or morphine after surgery - your brain adapts. Over time, it starts producing less of its own natural painkillers because the drug is doing the job. That’s normal. And if you suddenly stop? Your body panics.Withdrawal kicks in. Nausea. Vomiting. Sweating. Diarrhea. Anxiety. Yawning. These aren’t signs of being a bad person or losing control. They’re signs your nervous system is rewiring itself back to normal. Research shows 92% of people on long-term opioids get nausea during withdrawal. Almost 9 in 10 get anxiety. This isn’t addiction. It’s physiology.
The CDC says nearly everyone who takes opioids daily for more than 30 days becomes physically dependent. That’s not a failure. It’s expected. You don’t need to be judged for it. You just need to taper off safely.
What Addiction Actually Looks Like
Addiction - now called Opioid Use Disorder (OUD) - is not about withdrawal. It’s about loss of control. It’s when your brain’s reward system gets hijacked. You don’t take the drug because you need it for pain. You take it because your brain screams for it, even when you know it’s destroying your life.People with OUD often:
- Keep using even after losing their job, family, or housing
- Steal money or lie to get more pills
- Go to multiple doctors to refill prescriptions
- Feel intense cravings they can’t ignore
- Use opioids even when they’re causing harm - physically, emotionally, legally
These aren’t moral failures. They’re symptoms of a brain disease. Neuroimaging shows the prefrontal cortex - the part that controls decisions and impulses - is weaker in people with OUD. Their reward system is stuck on high. Even after years of sobriety, those changes linger.
Only about 8% of people prescribed opioids long-term develop OUD. That’s not a high number. But because so many people are prescribed these drugs, it still adds up to millions. And here’s the kicker: most of them never become addicted. They just become dependent. And that’s okay.
Why the Difference Matters
Confusing dependence with addiction has real-world consequences. A 2020 study found 68% of chronic pain patients thought withdrawal meant they were addicted. So they quit cold turkey - often in pain, scared, alone. Some even stopped taking medication their doctor prescribed because they were terrified of becoming an addict.Doctors, too, get it wrong. Fearing lawsuits or DEA scrutiny, some stop opioids abruptly when they see dependence. That’s dangerous. It can trigger severe withdrawal, worsen pain, and push people toward street drugs.
The CDC, the American Medical Association, and the National Institute on Drug Abuse all agree: physical dependence is not a reason to stop opioid therapy. If the drug is helping your pain and you’re not using it compulsively, you’re not addicted. You’re just dependent. And that’s manageable.
How to Tell Them Apart
Here’s a simple way to tell the difference:| Aspect | Physical Dependence | Addiction (Opioid Use Disorder) |
|---|---|---|
| Primary cause | Neurological adaptation to drug presence | Brain circuit changes affecting motivation and control |
| Key symptom | Withdrawal when drug stops | Compulsive use despite harm |
| Craving | Mild or absent | Intense, persistent, uncontrollable |
| Behavioral impact | No major life disruption | Job loss, relationship breakdown, legal trouble |
| Duration of brain changes | Resolves in weeks after stopping | Can last years, even after abstinence |
| Typical treatment | Gradual taper under medical supervision | Medication-Assisted Treatment (MAT) + counseling |
One patient on Reddit wrote: “I tapered off 60 mg of oxycodone a day over eight weeks. I had withdrawal for ten days - felt awful. But I never wanted to use it for fun. I just wanted to feel normal.” That’s dependence.
Another shared: “I stole from my mom. I drove two hours to get pills. I lost my job. I didn’t care. I just needed more.” That’s OUD.
What to Do If You’re Dependent
If you’ve been on opioids for more than a few weeks and your doctor says it’s time to stop, don’t quit cold turkey. Work with them on a taper. The CDC recommends reducing your dose by 5-10% every 2-4 weeks. If you’re on a high dose (over 100 morphine milligram equivalents per day), go slower - maybe 5% per month.Doctors use the Clinical Opiate Withdrawal Scale (COWS) to measure how bad withdrawal is. A score above 12 means you need help - maybe clonidine for anxiety, anti-nausea meds, or lofexidine, a newer FDA-approved drug specifically for opioid withdrawal.
Don’t be ashamed. This isn’t weakness. It’s a medical process. Thousands of people do this every year and go on to live full, healthy lives.

What to Do If You Have OUD
If you’re struggling with cravings, lying to get pills, or using despite consequences - you need more than a taper. You need Medication-Assisted Treatment (MAT).MAT isn’t trading one drug for another. It’s using FDA-approved medications - like buprenorphine or methadone - to stabilize your brain so you can focus on recovery. Studies show buprenorphine cuts death risk by 70-80%. Methadone cuts it by half.
Combine that with counseling, support groups, or therapy. You’re not broken. You’re sick. And like diabetes or hypertension, it’s treatable.
Insurance covers MAT. The Mental Health Parity Act requires it. If your provider says no, ask again. Or call SAMHSA’s helpline: 1-800-662-HELP. They’ll connect you to local programs.
The Bigger Picture
The opioid epidemic didn’t start because people got addicted to pain pills. It started because we told them they would. We made dependence look like a moral failure. We scared patients into quitting too fast. We made doctors afraid to help.Now we know better. We know that dependence is common. Addiction is rare. And both can be treated - but in totally different ways.
The FDA approved lofexidine in 2023. NIH is spending $1.8 billion on non-addictive pain treatments. New brain scans can now tell apart dependence from OUD with 89% accuracy. We’re getting closer to real solutions.
But until we stop calling dependence addiction, people will keep suffering in silence. They’ll keep being denied care. They’ll keep dying because we didn’t understand the difference.
You don’t have to be addicted to need help. And you don’t have to be dependent to be in danger. Understanding this isn’t just medical. It’s human.
Can you be physically dependent on opioids without being addicted?
Yes. In fact, most people who take opioids long-term for pain become physically dependent - about 90-100% of them. Physical dependence means your body adapts to the drug and experiences withdrawal if you stop suddenly. Addiction - or Opioid Use Disorder - means you lose control over your use, keep using despite harm, and have compulsive cravings. One is a normal biological response. The other is a brain disorder.
Does withdrawal mean I’m addicted?
No. Withdrawal is a sign of physical dependence, not addiction. If you take opioids for several weeks and then stop, you’ll likely experience nausea, sweating, anxiety, or diarrhea. That’s your body adjusting. Addiction involves compulsive drug-seeking behavior, lying to get prescriptions, using despite job loss or relationship damage, and intense cravings that override your judgment. Withdrawal alone doesn’t mean you have OUD.
How do doctors tell the difference between dependence and addiction?
Doctors use the DSM-5 criteria for Opioid Use Disorder, which includes 11 symptoms like cravings, loss of control, continued use despite harm, and neglecting responsibilities. If you have 2 or more in 12 months, it’s OUD. Physical dependence is diagnosed by the presence of withdrawal symptoms when the drug is stopped. They also use tools like the Opioid Risk Tool to assess your personal risk for addiction based on history, mental health, and family background.
Can I taper off opioids safely on my own?
It’s not recommended. Tapering too fast can cause severe withdrawal, increased pain, and even relapse. The CDC advises reducing your dose by 5-10% every 2-4 weeks, under medical supervision. If you’re on a high dose (over 100 MME/day), go slower - maybe 5% per month. Doctors can prescribe medications like clonidine or lofexidine to ease symptoms. Never quit cold turkey without professional support.
Is Medication-Assisted Treatment (MAT) just replacing one addiction with another?
No. MAT uses FDA-approved medications like buprenorphine or methadone to normalize brain chemistry, reduce cravings, and block the effects of other opioids. It’s not about getting high - it’s about restoring stability so you can rebuild your life. Studies show MAT cuts overdose deaths by up to 80%. It’s the gold standard of care for OUD, backed by decades of research. It’s treatment, not substitution.
Why do some doctors stop opioids abruptly if someone is dependent?
Many doctors confuse dependence with addiction out of fear - fear of legal trouble, DEA audits, or misjudging a patient’s risk. But this approach is harmful. The American Medical Association and CDC both warn against it. Abruptly stopping opioids can trigger severe withdrawal, worsen chronic pain, and push people toward illicit drugs. The right approach is to distinguish between dependence and addiction, then tailor treatment accordingly.
How common is Opioid Use Disorder among people prescribed opioids?
It’s relatively rare. Studies show only about 8% of patients prescribed opioids long-term for pain develop OUD. For people using opioids for acute pain - like after surgery - the risk is even lower, at 0.7-1%. Most people who take these medications as directed never become addicted. The bigger risk comes from misuse, mental health conditions, or a family history of substance use - not from taking the medicine itself.
What Comes Next
If you’re on opioids and worried about dependence, talk to your doctor about tapering. If you’re struggling with cravings or compulsive use, reach out for help. MAT works. Recovery is possible. And you don’t have to do it alone.Understanding the difference between physical dependence and addiction isn’t just about medical accuracy. It’s about giving people the care they deserve - without stigma, without shame, without fear.

This is such an important distinction. I had a friend taper off oxycodone after surgery and felt like a monster for needing help. Turns out she was just dependent. No judgment, just biology. Thank you for putting this out there.
So many people suffer in silence because they think they're weak. You're not.
Lmao this is peak woke medicine. 😂 Dependence? Addiction? Who cares. If you're takin' opioids, you're a junkie. The brain's a muscle, toughen up. 🤷♂️
It's critical to distinguish between physical dependence - a neuroadaptive response - and opioid use disorder, a chronic, relapsing brain disease characterized by compulsive use despite adverse consequences. The DSM-5 criteria are clear: two or more symptoms over 12 months constitute OUD. Withdrawal alone? That's physiological adaptation. Not pathology. Please, if you're reading this, understand: dependence ≠ addiction. This isn't semantics - it's clinical accuracy that saves lives.
Yessss!! This is the energy we need!! 💪 You're not broken if your body remembers what opioids did - you're human. And you deserve care, not stigma. I know someone who quit cold turkey because she thought she was 'addicted' - ended up in the ER with seizures. Please, if you're scared, reach out. You're not alone. We got you.
I’ve been on long-term opioids for fibromyalgia for 12 years. I’ve never used them for anything but pain. I’ve never lied, stolen, or chased highs. I’ve tapered slowly with my doctor’s help. I’m not addicted. I’m a patient. And I’m tired of being lumped in with people who misuse. This post is a lifeline.
I’m a nurse. I’ve seen this over and over. Patients crying because they’re terrified to ask for pain meds. Doctors refusing to refill because they’re scared of DEA audits. This isn’t healthcare - it’s fear-based triage. We need to stop punishing people for being sick. Dependence is normal. Addiction is treatable. Both deserve compassion. Not judgment. Period.
I was on 120mg oxycodone for 5 years after a car wreck. Tapered over 10 months. Withdrawal was brutal - but I never craved it for fun. I just wanted to stop feeling like I was drowning. People need to know: you can be dependent without being addicted. That’s not a weakness. That’s science.
This is so true. I used to think anyone on opioids was 'addicted' until my mom went through it. She was just dependent. She cried every day for two weeks. But she didn't steal from anyone. She didn't lie. She just wanted to feel okay. I wish more doctors knew this. 🙏
i had no idea this was a thing. i thought if u take em long u r a junkie. my uncle just stopped cold turkey and now he cant sleep or eat. i feel bad. thx for clarifying
I appreciate this breakdown. So many people don't realize that dependence is a biological response - not a character flaw. I’ve had patients panic because they felt 'sick' when they missed a dose. I always explain: your body is just recalibrating. It’s not addiction. It’s adaptation. And it’s temporary.
Look, I’ve been in recovery for 11 years. I know what addiction looks like. I know what it feels like to lie to your kids, to steal from your parents, to wake up and not care if you live or die. And I also know that most people on opioids aren’t like that. But here’s the thing - the system doesn’t care. Doctors still panic. Insurance still denies MAT. And people still die because we’re too scared to call it what it is. This post is right. But it’s not enough. We need systemic change - not just awareness. And until we fix that, the stigma will keep killing people. I’ve seen it. I’ve lived it. And I’m tired.
This is all propaganda. The CDC? The AMA? They’re all in bed with Big Pharma. They want you dependent so you keep buying pills. They’re lying about the 8% statistic - it’s actually closer to 40%. And lofexidine? That’s just another opioid in disguise. They’re trying to normalize addiction so they can profit. Don’t fall for it. If you take opioids, you’re already on the path to ruin. They just don’t want you to know it.
I'm sorry, but calling dependence 'normal' is dangerous. It's like saying 'it's normal to be drunk every night.' If your body adapts to a drug, that's a red flag - not a badge of honor. The fact that you're even asking if you're addicted means you're already in trouble.
The conflation of physiological adaptation with moral failure is indeed a profound societal failing. One must, however, acknowledge that the neurochemical alterations precipitated by chronic opioid exposure constitute a form of pathological reinforcement, regardless of behavioral manifestation. To label dependence as benign is to ignore the slippery slope inherent in pharmacological modulation of the mesolimbic pathway. One does not simply 'adapt' - one surrenders autonomy.
My dad was on pain meds for 15 years after a back injury. He never used them for anything else. He never lied. He never stole. He just wanted to walk without screaming. When his doctor cut him off because of 'risk,' he tried to kill himself. He didn’t want to die. He just didn’t want to live in pain. This isn’t about drugs. It’s about dignity. Thank you for saying this.