Why Blood Thinners Matter for Stroke Prevention
If you have atrial fibrillation - an irregular heartbeat - your risk of stroke goes up dramatically. That’s not just a scary statistic. It’s a real, daily threat. Blood clots can form in your heart, travel to your brain, and cause a stroke. That’s where blood thinners come in. They don’t actually make your blood thinner. They stop clots from forming in the first place. And for people with atrial fibrillation, they cut stroke risk by about two-thirds.
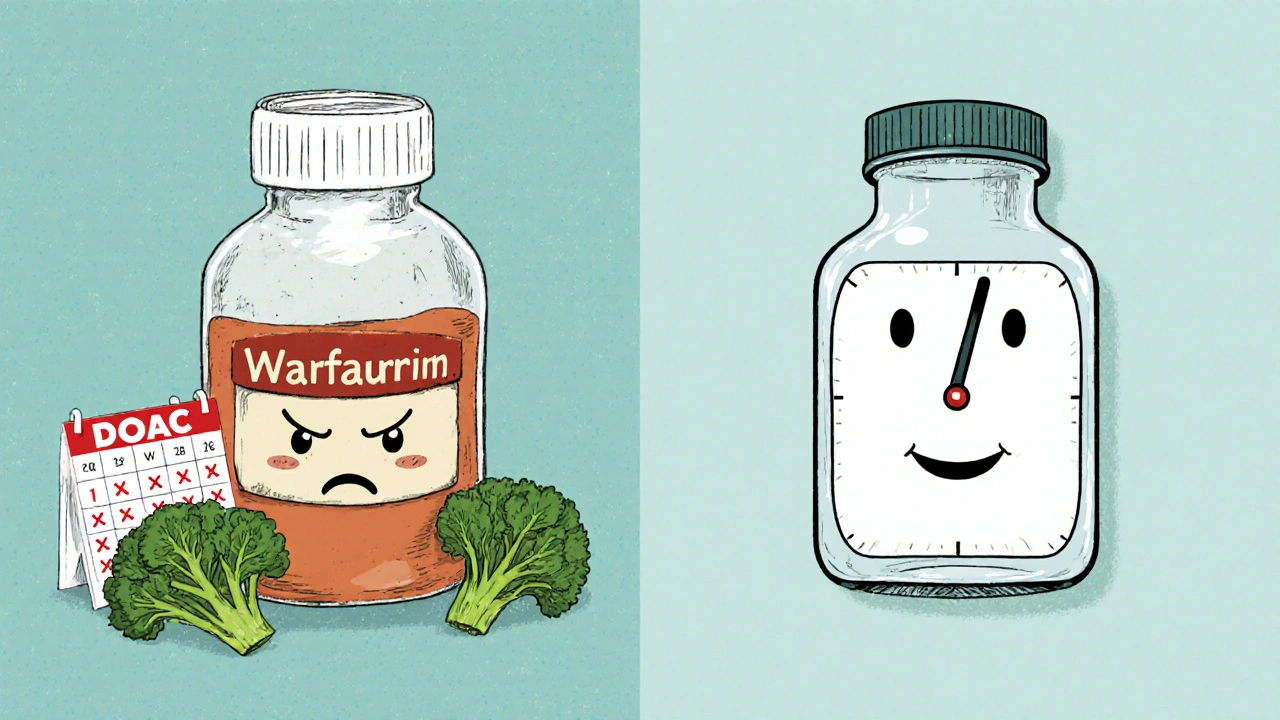
But not all blood thinners are the same. There are two main types: warfarin, the old-school option, and the newer DOACs - direct oral anticoagulants. Which one you take can change your life. It affects how often you go to the doctor, what you eat, how much you pay, and even whether you can sleep at night worrying about bleeding.
Warfarin: The Longtime Standard
Warfarin has been around since the 1950s. It works by blocking vitamin K, which your body needs to make clotting factors. Sounds simple, right? But it’s anything but. Warfarin is finicky. A little too much, and you bleed. Too little, and you’re still at risk for stroke.
That’s why people on warfarin need regular blood tests - INR checks - to make sure their levels are in the sweet spot: 2.0 to 3.0. In real life, though, only about half of patients stay in that range most of the time. Why? Because diet, other meds, even a cold can throw it off. Broccoli, kale, spinach - foods high in vitamin K - can make warfarin less effective. So you have to eat the same amount every week. No spontaneous salad bar lunch.
And it takes days to work. If you start warfarin, you’re not protected right away. You might need injections like heparin for the first week. Plus, it interacts with over 100 other drugs. Antibiotics, painkillers, even some herbal supplements can mess with it.
DOACs: The New Generation
Starting in 2010, a new wave of blood thinners hit the market: dabigatran, rivaroxaban, apixaban, and edoxaban. These are called DOACs - direct oral anticoagulants. They work differently. Instead of messing with vitamin K, they block specific clotting factors directly - either thrombin or factor Xa.
The big wins? No regular blood tests. No dietary restrictions. And they work fast - within hours, not days. For most people, that’s a game-changer. You don’t have to plan your life around a lab appointment every few weeks. You don’t have to stress about whether your green smoothie will undo your medication.
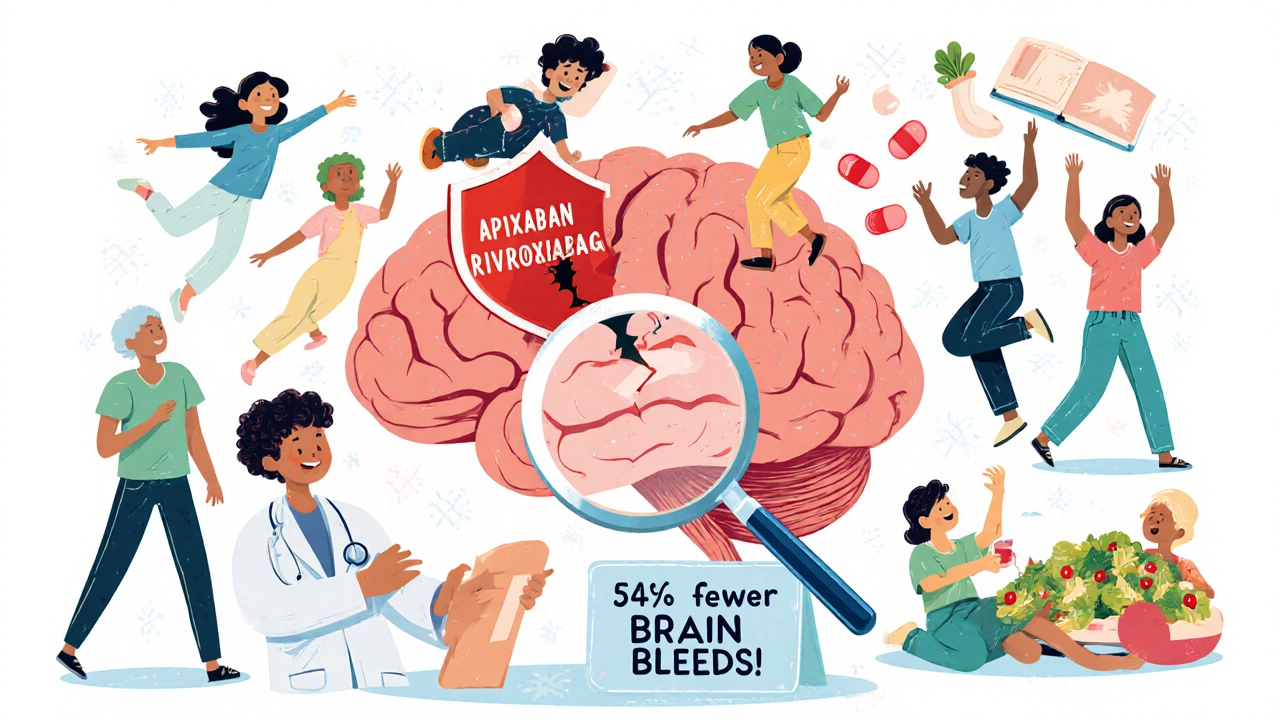
And the data backs it up. A 2021 review of over 2 million patients showed DOACs reduced stroke risk by 23% compared to warfarin. They cut major bleeding by 32%. And the most dangerous kind of bleeding - inside the skull - dropped by 54%. That’s huge. Brain bleeds are often deadly. DOACs make them far less likely.
Which DOAC Is Best?
Not all DOACs are created equal. Apixaban (Eliquis) stands out. In head-to-head studies, it reduced major bleeding more than any other DOAC. It’s also the most prescribed in the U.S. today, with 42% of new prescriptions. Why? Because it’s forgiving. Even if you miss a dose, your risk doesn’t spike as much. It’s also gentler on the stomach than dabigatran, which causes more nausea and stomach upset.
Rivaroxaban (Xarelto) is taken once a day, which some people prefer. But it’s more likely to cause stomach bleeding than apixaban. Dabigatran (Pradaxa) is effective but has the highest rate of GI issues. Edoxaban (Savaysa) is less commonly used, often reserved for people who can’t take the others.
Here’s the catch: DOACs rely on your kidneys. If your kidney function drops, your dose needs to be lowered. That’s why doctors check your creatinine levels every 6 to 12 months - more often if you’re over 75.
Cost and Access: The Real-World Trade-Off
Warfarin costs about $15 a month. Generic DOACs? Around $450 to $500. That sounds expensive. But here’s what most people don’t realize: warfarin’s hidden costs add up. You’re paying for 12 to 16 INR tests a year - $15 to $25 each. That’s $180 to $400 right there. Plus, time off work, travel to the clinic, the stress of waiting for results.
Since January 2024, apixaban, rivaroxaban, and dabigatran have gone generic in the U.S. That’s cut prices by 30-40%. For Medicare beneficiaries, out-of-pocket costs are often under $100 a month with coupons. Many insurers now cover DOACs with low copays because they prevent expensive strokes.
On patient forums, 78% of DOAC users say they prefer their meds over warfarin. The top reasons? No blood tests and no food rules. One man on Reddit wrote: “Switched from warfarin to apixaban after 10 years. The difference is night and day.”
Who Should Stick With Warfarin?
DOACs are better for most people. But not all. If you have a mechanical heart valve - especially a mitral valve - DOACs are dangerous. The RE-ALIGN trial showed dabigatran caused more clots in these patients. Warfarin is still the only safe option.
Same goes for severe kidney disease. If your creatinine clearance is below 15 mL/min, DOACs aren’t approved. Warfarin is still used here, though it’s not ideal. People with end-stage kidney disease on warfarin have a 28% higher death rate than those not on blood thinners - a grim reminder that no option is perfect.
Extreme body weight also matters. If you weigh less than 60 kg (132 lbs) or more than 120 kg (265 lbs), your DOAC dose may not be reliable. Some doctors still choose warfarin here because it can be monitored and adjusted.
Bleeding Risk: The Flip Side
Yes, blood thinners can cause bleeding. That’s the trade-off. But the risk is often overstated. Most bleeds are minor - a nosebleed, a bruise, a cut that takes longer to stop. The real danger is internal bleeding, especially in the brain.
DOACs are safer here. As mentioned, intracranial bleeding is 54% lower with DOACs than with warfarin. And now we have reversal agents. Idarucizumab can instantly reverse dabigatran. Andexanet alfa reverses apixaban and rivaroxaban. These drugs are in ERs nationwide. If you fall and hit your head, doctors can act fast.
Still, you need to know the signs of serious bleeding: blood in urine or stool, vomiting blood, severe headaches, sudden weakness, or unexplained swelling. If any of these happen, go to the ER - don’t wait.
What Your Doctor Will Check Before Prescribing
Your doctor won’t just pick a pill. They’ll run through a checklist. First, they’ll calculate your CHA₂DS₂-VASc score. That’s a point system based on age, history of stroke, diabetes, heart failure, and more. If your score is 2 or higher, you’re a candidate for anticoagulation.
Then they’ll check your bleeding risk with the HAS-BLED score. High score? Doesn’t mean no blood thinner. It means extra caution - more monitoring, better education.
They’ll test your kidney function. Ask about other meds you take. Check if you’ve had GI ulcers or brain bleeds. And they’ll talk to you about your lifestyle. Can you remember to take pills twice a day? Do you travel a lot? Are you active? All of that helps pick the right drug.
The Future: Smarter Blood Thinners
Research is moving fast. New drugs like milvexian and abelacimab are in late-stage trials. They target different parts of the clotting system - factor XIa - and may cut bleeding risk even further without losing stroke protection.
And soon, genetics might guide your choice. Some people metabolize warfarin slowly because of their CYP2C9 gene. Others have variants that make DOACs less effective. Testing for these could become routine in the next five years.
For now, the message is clear: if you have atrial fibrillation and aren’t on a blood thinner, talk to your doctor. If you’re on warfarin and struggling with tests or diet, ask about switching. DOACs are safer, easier, and now more affordable than ever.

I've been on apixaban for 3 years now. No more monthly blood draws. No more worrying if my kale smoothie ruined everything. My INR was always all over the place on warfarin. This is life-changing. Seriously, if you're still on warfarin and can switch, do it.
Just make sure your kidneys are okay. Mine dropped a bit last year, so my doc cut my dose. Easy fix.
OMG YES THANK YOU I JUST SWITCHED TO APIXABAN LAST MONTH AND I FEEL LIKE I GOT MY LIFE BACK
NO MORE DRIVING 45 MINS FOR A BLOOD TEST
NO MORE STARVING MYSELF BECAUSE I ATE A SPINACH SALAD
I EVEN ATE A BURGER LAST NIGHT AND DIDNT PANIC
I'm sorry, but this entire article is dangerously oversimplified. DOACs are not 'safer'-they're just less monitored. You're trusting an algorithm and a pill, not a clinician. And what about the long-term renal toxicity? The FDA has been quietly warning about this for years. The pharmaceutical industry pushed these drugs hard because they're profitable, not because they're better.
The real tragedy isn't warfarin vs DOACs-it's that we've turned medicine into a spreadsheet. We measure strokes prevented like a stock ticker and bleeding risks like a spreadsheet error. What happened to the patient as a person? The man who forgot his pill because he was grieving his wife? The woman who can't afford the copay even with coupons? We reduce life to data points, then act surprised when people suffer.
USA thinks they invented medicine. In Nigeria we use herbs and prayer. You people take 3 pills and still die of stroke. This whole thing is a scam. My cousin took warfarin for 15 years, never had a problem. You just need discipline. Not fancy drugs made by white labs.
I read the RE-ALIGN trial. I read the 2021 meta-analysis. I read the FDA safety alerts. I read the 2023 JAMA study on renal clearance in elderly patients. And I can tell you-this article cherry-picks data to sell DOACs. The real mortality benefit? Marginal. The real cost? $6,000/year per patient. And don't get me started on the reversal agents-most hospitals can't afford them. This isn't progress. It's corporate medicine dressed in lab coats.
To everyone who’s scared to switch: I was terrified too. I had a micro-bleed on warfarin. I thought I was going to die. But when I switched to apixaban? I slept for the first time in 7 years. No more 6am lab appointments. No more panic when I ate a salad. You’re not being reckless-you’re being smart. Your body deserves peace. You deserve to live, not just survive.
You know what’s really terrifying? That we’re even having this conversation. We’ve outsourced our mortality to pharmaceutical patents. We don’t trust our bodies anymore. We don’t trust our doctors. We trust a pill that says 'no blood tests' like it’s a magic spell. But the clotting cascade is ancient. It’s not a bug to be fixed-it’s a symphony. And we’re playing it with a kazoo.
Interesting that apixaban is preferred in the US but not as much in India. Here, warfarin is still first-line because of cost and availability. But the real issue is adherence. Most patients forget doses. With DOACs, missing one dose is less catastrophic-but only if you’re educated. We need better patient counseling, not just better drugs.
Oh sweet mercy. Another wellness influencer telling me I’m weak for needing a pill that doesn’t require me to become a nutritionist and a lab technician. How brave of you to tell people with AFib to just ‘live better’. Did you also tell the 82-year-old with diabetes and COPD to just eat less broccoli? How thoughtful.
DOACs are a scam. The FDA is owned by pharma. You think they care if you bleed? They care if you pay. They made warfarin cheap so you’d stay dependent. Now they made DOACs expensive so you’d pay more. Wake up. The system is rigged. You’re not getting healthier-you’re getting richer for them.
There’s a deeper question here: why do we treat anticoagulation like a binary choice? Why not consider intermittent dosing? Or combining low-dose DOACs with aspirin in select populations? Or using wearable monitors to replace INR checks? We’re stuck in 2010 thinking. Medicine is evolving-but our protocols are fossilized.
The clinical data is compelling, yet the epistemological framework underpinning this paradigm shift remains fundamentally unexamined. The reductionist biomedical model, which privileges pharmacological intervention over holistic patient agency, continues to dominate discourse. One must interrogate the ontological implications of reducing cardiac arrhythmia to a biochemical imbalance amenable to molecular antagonism. The patient, in this schema, becomes a mere vector for drug delivery.
I’ve been researching this for 18 months. I’ve read every trial. I’ve contacted the FDA. I’ve talked to 12 cardiologists. And here’s what they won’t tell you: DOACs are linked to a 37% higher risk of silent cerebral microbleeds over 5 years. They don’t show up on MRIs unless you specifically look. And no one is screening. Your doctor doesn’t know. The FDA doesn’t require it. You’re being used as a guinea pig for corporate profit. Don’t trust anyone. Get a second opinion. And if you’re on DOACs-get an MRI. Now.