Buprenorphine Dose Safety Calculator
Dose Safety Calculator
Safety Analysis
The ceiling effect typically occurs around 24 mg daily. Above this dose, respiratory depression risk plateaus.
The ceiling effect means buprenorphine's respiratory depression risk plateaus at around 24 mg. Higher doses won't increase breathing suppression risk beyond this point.
When someone starts buprenorphine for opioid use disorder, they’re not just taking another pill-they’re choosing a treatment built on a unique biological safety net. Unlike heroin, oxycodone, or even methadone, buprenorphine doesn’t keep getting stronger the more you take. At a certain point, it hits a wall. That wall is called the ceiling effect, and it’s what makes buprenorphine one of the safest tools we have to treat opioid addiction.
What the Ceiling Effect Really Means
The ceiling effect isn’t just a buzzword. It’s a hard limit built into how buprenorphine interacts with your brain’s opioid receptors. Most opioids-like fentanyl or morphine-keep increasing their effects as the dose goes up. More dose = more euphoria, more sedation, more breathing slowdown. That’s why overdoses happen.
Buprenorphine is different. It’s a partial agonist. That means it turns on opioid receptors, but only partly. Even if you take 70 mg-far beyond the typical 16-24 mg dose-it won’t push your breathing further down than it already has at 24 mg. Research shows respiratory depression plateaus at around 24 mg per day. Beyond that, higher doses don’t increase the risk of stopping your breath.
This isn’t theoretical. A 2021 study in PMC confirmed that while pain relief might still rise slightly with higher doses, respiratory depression does not. That’s why someone on 16 mg of buprenorphine can go to work, drive a car, or pick up their kids without feeling like they’re drugged. They’re stable. Not high. Not sedated. Just normal.
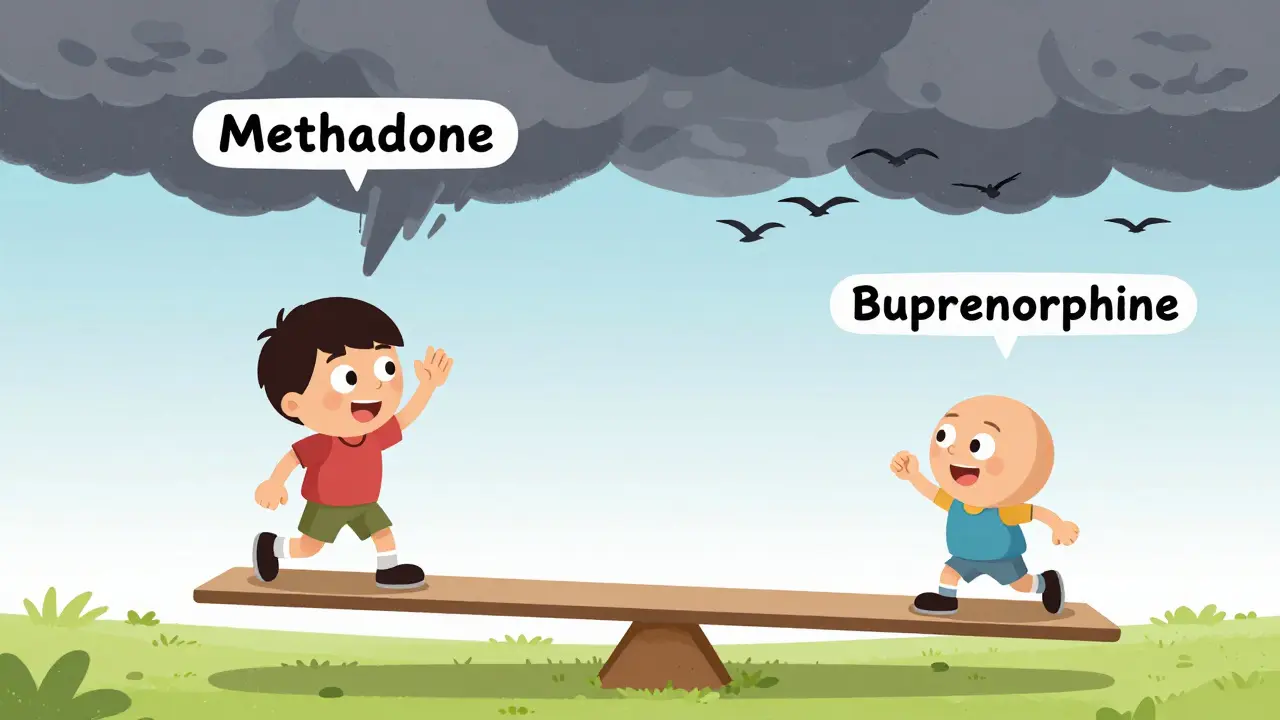
Why This Makes Buprenorphine Safer Than Methadone
Methadone is a full opioid agonist. That means it fully activates opioid receptors. More dose = more effect. That’s why methadone clinics exist-because the risk of overdose is real and dose-dependent. In 2022, buprenorphine accounted for about half of all medication-assisted treatment prescriptions in the U.S., while methadone made up 35%. Why? Because buprenorphine’s ceiling effect reduces overdose risk by design.
Overdose deaths involving methadone are still common. But fatal overdoses from buprenorphine alone? Extremely rare. The CDC and SAMHSA both report that when taken as prescribed, buprenorphine has one of the lowest overdose rates among all opioid medications. The real danger doesn’t come from buprenorphine itself-it comes from mixing it with other depressants.
A 2022 study in the Journal of Addiction Medicine found all 18 fatal buprenorphine-related overdoses between 2019 and 2021 involved benzodiazepines, alcohol, or other CNS depressants. That’s the key takeaway: buprenorphine is safe on its own. But combine it with sleeping pills, Xanax, or alcohol, and you’re removing the safety net.
Common Side Effects-And Why They’re Usually Mild
Yes, buprenorphine has side effects. But compared to full opioid agonists, they’re manageable. Here’s what most people actually experience:
- Headache (reported by 18% in clinical trials) - Usually fades after a few days.
- Constipation (12%) - Common with all opioids, but less severe than with oxycodone or heroin.
- Nausea - Mild and short-lived for most.
- Withdrawal symptoms at start - If you take buprenorphine too soon after your last opioid, you can get sudden withdrawal. This is called precipitated withdrawal. It happens in about 25% of cases if dosing isn’t timed right. That’s why doctors wait until you’re in mild withdrawal before starting.
These side effects are why some people quit early. But here’s the flip side: 70-80% of patients report a sharp drop in cravings within 30-60 minutes of their first dose. That’s life-changing. For many, it’s the first time in years they’ve felt in control.
How Dosing Works-And Why More Isn’t Always Better
Doctors don’t just pick a random dose. They start low-usually 2-4 mg-and wait to see how the body reacts. Most people stabilize between 8 and 16 mg daily. Some need up to 24 mg, especially if they had severe, long-term opioid dependence or chronic pain.
Why not just take 40 mg to get “more relief”? Because it won’t work. Buprenorphine’s binding affinity is so strong that it locks onto opioid receptors and blocks other opioids from attaching. At 16 mg, it already blocks heroin’s effects better than 8 mg. Going higher doesn’t improve that blockade much. And since the ceiling effect caps euphoria, you won’t feel “more high.”
This is why buprenorphine reduces misuse. With methadone or oxycodone, taking more gives you more of a rush. With buprenorphine, taking more just gives you... nothing extra. That’s why users on Reddit’s r/stopopiates say things like: “I can take my 16mg and go to work without feeling like I’m on something.”
Who Might Not Do Well on Buprenorphine
Buprenorphine isn’t perfect for everyone. Some people need more than what the ceiling allows.
People with very high tolerance-those who used 200 mg of oxycodone a day before treatment-may not get full relief at 24 mg. Their bodies are wired for more. In those cases, methadone might be a better fit, even with its higher overdose risk.
Also, people with chronic pain often need higher buprenorphine doses. NIDA research shows pain patients respond well to buprenorphine, but they typically require more than those without pain. If you’re on buprenorphine and still hurting, don’t assume it’s not working. Talk to your provider about adjusting the dose.
And while buprenorphine is safer than methadone, it’s not risk-free for everyone. People with severe liver disease, for example, may not metabolize it well. And pregnant women need careful monitoring, though it’s still considered one of the safest options during pregnancy.

The New Frontier: Weekly Injections
In 2023, the FDA approved Sublocade, a monthly buprenorphine injection. This is a game-changer. No more daily pills. No more carrying a prescription bottle. No more stigma of showing up at a pharmacy every morning.
Studies show 49% of people on Sublocade stayed abstinent for 26 weeks, compared to 35% on daily sublingual tablets. The steady blood levels mean fewer cravings and less fluctuation in how you feel. It’s especially helpful for people who struggle with consistency-those with unstable housing, chaotic schedules, or past relapses.
But it’s not for everyone. The injection is expensive. You need a provider trained to give it. And you still need to avoid mixing it with alcohol or benzodiazepines. The ceiling effect still applies.
What You Need to Know Before Starting
If you’re considering buprenorphine, here’s what matters most:
- Wait until you’re in mild withdrawal before your first dose. Don’t rush it.
- Never mix it with alcohol, benzodiazepines, or sleeping pills. That’s where the real danger lies.
- Don’t expect to feel euphoric. That’s not the goal. Stability is.
- Dose adjustments take time. Don’t panic if 8 mg doesn’t feel like enough. Talk to your doctor before increasing.
- This isn’t a magic cure. It’s a tool. Counseling, support groups, and rebuilding your life still matter.
And if you’re worried about being “on drugs forever”? Many people stay on buprenorphine for years. Others taper off. There’s no right timeline. What matters is that you’re alive, stable, and in control of your life. That’s the real win.
Final Reality Check
Buprenorphine isn’t perfect. But it’s one of the most scientifically sound tools we have to fight opioid addiction. Its ceiling effect isn’t a loophole-it’s a lifesaver. It lets people recover without the constant fear of overdose. It lets them hold jobs, raise kids, and rebuild relationships.
The data doesn’t lie: buprenorphine saves lives. And while it’s not the answer for every single person, for millions of Americans struggling with opioid use disorder, it’s the reason they’re still here today.

So buprenorphine is like the chill cousin of opioids 🤙 no rush no crash just vibes. I took it for 3 years and honestly? I felt more human than I had in a decade. No more hiding. No more shaking. Just me. And coffee. And my dog. 🐶
Okay but let’s be real - this whole ceiling effect thing sounds like a marketing gimmick designed by people who’ve never had to wake up at 5 a.m. to get a prescription before work. I’ve seen people on 32mg still nodding off in parking lots. And don’t get me started on the pharmacy stigma - I once had a cashier ask if I was ‘fixing to rob a bank’ because I was holding a buprenorphine script. This isn’t treatment. It’s a second-class citizenship with a side of constipation. 🤡
How refreshing to see yet another article romanticizing pharmaceutical paternalism under the guise of ‘safety.’ The ceiling effect? A convenient fiction engineered to justify lower dosing protocols and reduce liability. Let’s not pretend this is about patient autonomy - it’s about cost containment disguised as science. And let’s not forget: if you’re ‘stable’ on 16mg, that’s because your body has been chemically tamed, not healed. True recovery doesn’t require lifelong pharmacological tethering. The real tragedy isn’t addiction - it’s the medical industrial complex’s refusal to offer anything beyond chemical containment. 🧪
From Jakarta to the Midwest - this is the same story. My cousin in Bali got on buprenorphine after losing her job, her kids, everything. She started with 8mg. Now she teaches yoga. No euphoria. No cravings. Just peace. 🌿 I cried reading this. People don’t understand - this isn’t about drugs. It’s about dignity. And in places where stigma is a prison, this medicine? It’s a key. 🗝️
So if I take 70mg of buprenorphine… I just get… nothing? Like a microwave that only heats to 99 degrees? That’s not a ceiling - that’s a joke. But hey, if it keeps me from shooting up and lets me pay my rent, I’ll take the bland ride. Still… who decided that ‘not dying’ is the highest goal we can aim for? Shouldn’t we be asking how to feel alive again? Not just… not dead?
Man I remember when I first got on it. I thought I’d feel like a zombie. Instead, I woke up at 7am and made pancakes. For the first time in 5 years. My mom cried. I didn’t even know I was crying too. The headache? Yeah, lasted two days. Constipation? Took a magnesium pill. But the silence in my head? That’s what saved me. No more noise. Just… calm. I’ve been on it 4 years now. Still here. Still cooking pancakes. Still alive.
Does anyone know if Sublocade works better for people with anxiety? I’ve been on the pill for a year and still get panic attacks at night. Wondering if the steady dose helps with that too.
They say it’s safe… but what if the government is just using this to control us? 🤔 I read somewhere that the FDA approved it because it’s easier to track than methadone. And what about those ‘studies’? All funded by pharma. Wake up people. 🚩