Isotretinoin Mental Health Risk Assessment
Personalized Risk Assessment
This tool estimates your risk of mood changes during isotretinoin treatment based on clinical data. It's not medical advice—always discuss results with your dermatologist.
Check all that apply:
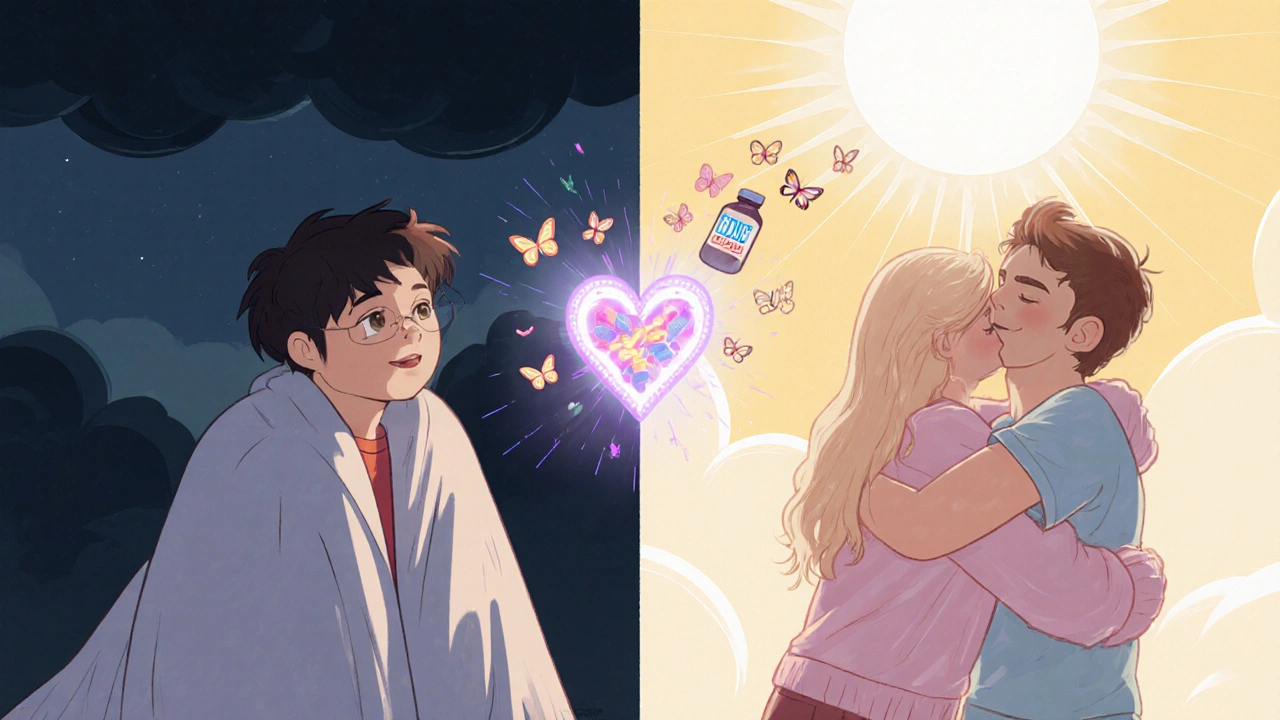
Isotretinoin works wonders for severe acne-85% of people see long-term clearance after one course. But for some, the clear skin comes with a hidden cost: mood changes, anxiety, or even depression. If you’re considering isotretinoin, or already on it, understanding the real risks and how to monitor them isn’t optional-it’s essential.
Is There a Real Link Between Isotretinoin and Depression?
The answer isn’t simple. On one side, the FDA has tracked over 19,000 reports of psychiatric side effects linked to isotretinoin since 2004. Depression showed up in nearly half of those cases. Suicidal thoughts were reported more than 11 times more often than in people not taking the drug. These aren’t random anecdotes-they’re data from a national database used by doctors and regulators.
But here’s the twist: a massive 2023 study of over 1.6 million people found no higher risk of suicide or depression in isotretinoin users compared to the general population. The 1-year risk of suicide attempt? Just 0.14%. That’s lower than the baseline rate in teens without acne. The same study showed depression occurred in 3.83% of users-right in line with typical rates for adolescents.
So why the contradiction? One big clue: people with pre-existing mental health conditions are at higher risk. If you’ve had depression, anxiety, or suicidal thoughts before, isotretinoin may make things worse. And the timing matters. Most mood changes show up around week 8-give or take a few weeks. That’s not a coincidence. It’s a pattern.
Who’s Most at Risk?
Not everyone is equally vulnerable. Three factors stand out:
- History of mental health issues-This is the biggest red flag. If you’ve ever been diagnosed with depression, bipolar disorder, or had suicidal thoughts, your risk jumps. The JAMA Dermatology study showed these patients had significantly higher chances of psychiatric events.
- Age and gender-Older patients (over 25) had lower rates of depression. Men were more likely to report completed suicide attempts, which matches broader trends in suicide epidemiology.
- Dose matters-but not how you think-Higher cumulative doses were linked to *lower* risk of suicide attempts. That doesn’t mean more is safer. It suggests people who tolerate higher doses may have fewer underlying vulnerabilities.
And don’t forget: acne itself can cause depression. Many patients report feeling better mentally once their skin clears. That makes it hard to tell if mood changes come from the drug-or from the relief of finally feeling seen again.
What the Experts Say
Doctors aren’t ignoring this. The American Academy of Dermatology (AAD) updated its guidelines in 2022 to say: monitor, don’t avoid. They recommend a baseline mental health check before starting isotretinoin. That means asking about past depression, family history, current meds, and any recent stressors.
The FDA’s iPLEDGE program, which all prescribers must follow, now requires monthly screening using the PHQ-9-a simple 9-question depression checklist. If your score hits 10 or higher, you must see a mental health professional before getting your next prescription.
Some clinics have gone further. UCSF’s protocol now includes a mandatory “mental health pause” at week 8. No refills until you’ve had an in-person check-in. That’s not overkill-it’s smart. Because 44% of psychiatric events happen in those first eight weeks.
What to Watch For
You don’t need to be a psychiatrist to spot trouble. Here’s what to look out for:
- Emotional blunting-Feeling numb, detached, or like you’ve lost interest in things you used to enjoy.
- Increased irritability-Getting angry over small things, snapping at loved ones, feeling on edge.
- Sudden sadness-Crying for no clear reason, feeling hopeless, or saying things like “What’s the point?”
- Sleep and appetite changes-Sleeping too much or too little, losing interest in food, or binge-eating.
- Suicidal thoughts-Any mention of wanting to die, feeling like a burden, or making plans to end your life. This is an emergency.
If you notice any of these-especially the last one-stop the medication and call your doctor immediately. Don’t wait. Don’t talk yourself out of it. Your mental health matters as much as your skin.
What About Other Acne Treatments?
Isotretinoin isn’t the only option. Antibiotics like doxycycline and minocycline are common, but minocycline has its own mental health risks-about 1.7% of users report depression. Topical retinoids like tretinoin rarely affect mood. Light therapy and hormonal treatments (for women) are other alternatives.
But here’s the truth: isotretinoin is still the most effective treatment for severe, scarring acne. If other options failed, it’s often the only path to lasting results. The question isn’t whether to avoid it-it’s how to use it safely.
Real Stories, Real Concerns
Reddit’s r/Accutane community has 147,000 members. In a July 2024 thread, 43% reported worsening depression or anxiety. One user wrote: “Week 8 brought severe depression I’d never experienced before-constant crying, loss of interest in everything. I stopped and symptoms vanished in three weeks.”
But others say the opposite: “My depression lifted dramatically on isotretinoin-my acne was the root cause.” That’s the paradox. For some, the drug causes distress. For others, it’s the cure.
On Drugs.com, isotretinoin has a 5.5/10 rating. 38% of reviews cite mental health as a negative. But 22% say it improved their quality of life. The difference? Often, whether they were screened before starting-and whether they had support.
What’s Changing in 2025?
The rules are getting stricter-and smarter. Starting January 1, 2025, every doctor prescribing isotretinoin in the U.S. must complete 2 hours of mental health training annually. Skip it, and they lose their iPLEDGE access.
The FDA is also piloting digital PHQ-9 check-ins through the iPLEDGE app. Instead of waiting for a monthly visit, you’ll get a quick survey every week during the first two months. It’s not invasive-it’s preventive.
And new research is pointing to genetics. A July 2024 study found a specific gene variant (BDNF Val66Met) may predict who’s more likely to develop depression on isotretinoin. The test is still experimental, but it’s a step toward personalized care.
Your Action Plan
If you’re considering isotretinoin, here’s what to do:
- Get screened before starting-Ask your dermatologist for a PHQ-9 or Beck Depression Inventory. Be honest. No judgment.
- Share your history-Tell them about past depression, anxiety, therapy, or medication. Even if it was years ago.
- Set up weekly check-ins-Even if your doctor doesn’t require it, schedule them. Call a friend, journal your mood, or use a free app like Moodfit.
- Watch for red flags-Especially between weeks 4 and 10. If something feels off, speak up.
- Know your exit plan-If you feel worse, stopping isotretinoin is safe. Symptoms usually fade within weeks.
Clear skin is important. But your mind matters more. You don’t have to choose between them.
What If You’re Already on Isotretinoin?
If you’re already taking it:
- Don’t panic. Most people don’t have issues.
- Check your last PHQ-9 score. If it’s been over a month, ask for a new one.
- Call your doctor if you’ve had any mood changes-even if you think it’s “just stress.”
- Don’t stop cold turkey unless you’re in crisis. Talk to your provider first.
And if you’re feeling isolated? You’re not alone. Thousands are going through the same thing. Support groups, online forums, and even your dermatologist’s office can connect you with others who get it.
Can isotretinoin cause suicide?
Isotretinoin has been linked to suicidal thoughts in rare cases, but studies show the absolute risk is very low-about 0.14% in one year. That’s lower than the suicide attempt rate in teens without acne. However, people with a history of depression or suicidal ideation are at higher risk. Any mention of suicide or self-harm requires immediate medical attention and discontinuation of the drug.
How often should I be screened for depression while on isotretinoin?
The iPLEDGE program requires monthly screening using the PHQ-9. But experts recommend more frequent checks during the first 8 weeks, when most mood changes occur. Weekly digital check-ins or in-person visits every 2 weeks during this time are considered best practice. If your PHQ-9 score is 10 or higher, you must be evaluated by a mental health professional before continuing treatment.
Should I avoid isotretinoin if I’ve had depression before?
Not necessarily. Many people with past depression take isotretinoin safely with close monitoring. The key is full disclosure-tell your dermatologist your history, get a baseline mental health assessment, and agree on a monitoring plan. Studies show that patients with prior psychiatric conditions are at higher risk, but that risk can be managed with regular check-ins and early intervention.
Do I need a psychiatrist to prescribe isotretinoin?
No. Dermatologists can prescribe isotretinoin. But they must follow the iPLEDGE program, which includes mental health screening. If you have a complex psychiatric history, your dermatologist may refer you to a psychiatrist for evaluation before starting. You don’t need a psychiatrist to prescribe it, but you may need one to help manage your care.
How long do depression symptoms last after stopping isotretinoin?
For most people, mood changes improve within 2 to 6 weeks after stopping isotretinoin. In reported cases, symptoms like sadness, irritability, or emotional numbness often resolve completely. If symptoms persist beyond 6 weeks, it’s likely unrelated to the medication and should be evaluated as a separate mental health condition.
Can vitamin B12 deficiency cause similar symptoms?
Yes. A 2022 study found that 18.7% of isotretinoin users develop vitamin B12 deficiency, which can cause fatigue, depression, and brain fog. Many clinics now check B12 levels before and during treatment. If your mood changes coincide with low B12, supplementation can help-without stopping isotretinoin.
Are there any genetic tests to predict if I’ll get depressed on isotretinoin?
An experimental test for a gene variant called BDNF Val66Met shows promise-it correctly identified 68% of people who later developed depression on isotretinoin. But it’s not yet available outside research settings. For now, your personal and family mental health history is the best predictor.
Next Steps
If you’re thinking about isotretinoin: talk to your dermatologist. Ask for the PHQ-9. Share your full mental health history. Don’t be afraid to push for more frequent check-ins. You’re not overreacting-you’re being responsible.
If you’re already on it: don’t ignore your mood. Track it. Talk about it. Reach out if something feels wrong. Clear skin shouldn’t cost your peace of mind.
Isotretinoin is powerful. It changes lives. But only if you use it with awareness-not fear, not denial, but thoughtful, informed care.

Been on isotretinoin for 6 months. My skin cleared up, but I felt like a ghost for a while-no joy in anything, even my favorite games. Stopped at week 9, and within 10 days, I was myself again. Not saying it’s bad for everyone, but if you’re feeling off, don’t brush it off as ‘just stress.’ Your brain matters more than your face.
Also, B12 check? My doc didn’t mention it. Got tested anyway-low as hell. Supplemented, and my brain fog lifted. Maybe that’s what was really going on.
Oh great. So now we’re treating acne like it’s a nuclear launch code. ‘Oh no, the magic pill might make you sad? Better schedule a therapy session, fill out 17 forms, and meditate with a crystal while your face peels off.’
Meanwhile, my cousin got prescribed doxycycline and developed a yeast infection, but nobody’s writing a 3,000-word essay about ‘microbiome trauma.’ Hypocrisy is a beautiful thing.
While I appreciate the thoroughness of this post, I must respectfully underscore the methodological nuances between pharmacovigilance data and population-level epidemiological studies. The FDA’s spontaneous reporting system is inherently biased toward adverse event ascertainment, whereas the 2023 cohort study controlled for confounders such as baseline psychological distress and acne severity.
That said, the clinical imperative remains: personalized risk stratification is not optional. The BDNF Val66Met polymorphism, though not yet clinically validated, represents a paradigm shift toward pharmacogenomic-guided dermatology. I urge all prescribers to consider baseline PHQ-9 and B12 levels as standard of care-not as bureaucratic hurdles, but as ethical obligations.
WAIT WAIT WAIT-so you’re telling me I could’ve avoided 3 months of crying and hating my reflection just by checking my B12?? My doctor didn’t even BOTHER to test it!! I was convinced I was broken!! I took it because I thought my acne was making me depressed-but what if it was just my body starving for B12??
And why is this not common knowledge?? I’ve seen 3 dermatologists and NO ONE said a word!! This is insane!! I feel like I was lied to!!
Also, why is the FDA letting doctors skip mental health training?? I’m reporting this!!
from india here, my cousin took isotretinoin and she was fine, no mood issues. but she had strong family support, talked to her mom every day, and went for walks. maybe it’s not just the drug, but how alone you feel while taking it?
i read this whole thing and i’m glad someone finally said it: clear skin doesn’t fix loneliness. if you’re isolated, even the best treatment can feel like a trap.
also, check your vit d and b12. in india, so many of us are low and no one ever tests it. just saying.
The tragedy isn’t the drug-it’s the cultural delusion that physical perfection is the only path to self-worth. We’ve been conditioned to believe that flawless skin is synonymous with being lovable, successful, worthy. Isotretinoin doesn’t cause depression; it exposes the hollowness of the myth we’ve been sold. When your skin clears and you’re still empty inside… what then? The drug didn’t break you. The system did.
And now we’re reduced to debating PHQ-9 scores and B12 levels like they’re magic bullets. We’ve turned healing into a checklist. We’ve outsourced our humanity to algorithms and blood tests. And we wonder why people still feel alone.
The real question isn’t whether isotretinoin causes depression. It’s why we think we need to be beautiful to be safe.
And that… that’s the real epidemic.
Oh look, another person who thinks their feelings are more important than their skin. You want to be emotionally safe? Don’t take a drug that makes you look like a human again. Just stay pimple-faced and call it ‘authentic.’
Meanwhile, people who actually had real depression-like, clinical, suicidal, therapy-and-medication-level depression-are being gaslit by people who think crying over acne is a trauma narrative. Grow up. The world doesn’t owe you emotional comfort just because you want to look like a model.
And yes, I’ve been on it. I didn’t cry. I got my confidence back. Deal with it.
bro i took isotretinoin in 2021 and my skin went from ‘ugly kid in class photo’ to ‘whoa dude who’s that’
but yeah week 7 i just sat on my bed staring at the wall for 3 days
didn’t tell anyone cause i thought i was being dramatic
then i stopped and boom-woke up laughing at memes again
also my b12 was low as f***
so yeah maybe it’s not the drug maybe it’s the combo of being alone in a dorm room with no one to talk to and your body being low on vitamins
just saying
I was on it for 7 months. Didn’t feel depressed. But I did feel… empty. Like I’d been waiting so long to feel good about my face, that when it finally happened, I didn’t know what to do with myself. I didn’t know who I was without the acne.
It wasn’t sadness. It was confusion.
And nobody talks about that.
This is one of the most balanced, thoughtful pieces I’ve read on this topic. Thank you for including the nuance-the data, the stories, the alternatives, the science. So many posts on this either fearmonger or dismiss entirely.
As someone who’s had both acne and anxiety, I can say: I needed this treatment. But I also needed the weekly check-ins. I needed my therapist to know I was on it. I needed to know it was okay to stop.
It’s not an either/or. It’s a both/and. Skin and soul. Both matter.
Interesting how the FDA’s iPLEDGE system treats isotretinoin like a controlled substance. Yet we hand out SSRIs like candy. The irony is thick.
Also, the BDNF gene study? Fascinating. But if we’re going to personalize treatment, why not start with the low-hanging fruit-like checking B12 before prescribing? Simple, cheap, effective. Why make it complicated?